The immune system’s ability to recognize and destroy cancer cells is often thwarted by tumors that evolve sophisticated evasion mechanisms. Traditional immunotherapies, such as checkpoint inhibitors, work by removing these brakes on immunity, but they lack precision and can trigger systemic autoimmunity. Molecular glue degraders, exemplified by compounds like PVTX-405, represent a paradigm shift—small molecules that force pathogenic proteins into the cell’s natural degradation machinery, effectively erasing them from existence. Unlike PROTACs, which require a bulky bifunctional structure, molecular glues operate with elegant minimalism, hijacking E3 ubiquitin ligases to mark oncoproteins for destruction. This emerging class of drugs is redefining targeted immunotherapy, offering a way to dismantle cancer’s defenses at the molecular level without collateral damage.
The Rise of Molecular Glues: From Serendipity to Rational Design
The discovery of molecular glue degraders began with unexpected observations. Thalidomide, once infamous for its teratogenic effects, was later found to bind cereblon, an E3 ligase, and degrade transcription factors like IKZF1/3 in multiple myeloma. This accidental insight revealed that small molecules could induce protein-protein interactions that would never occur naturally, coercing the ubiquitin-proteasome system to eliminate disease-causing proteins. Scientists quickly recognized the therapeutic potential of this mechanism, sparking a wave of research into synthetic molecular glues.
Unlike traditional inhibitors, which merely block protein activity, degraders remove the target entirely. This is particularly advantageous in oncology, where compensatory pathways often render inhibitors ineffective over time. PVTX-405, a cereblon-based glue, exemplifies this principle by degrading the immunosuppressive factor PD-L1 directly within tumor cells, preventing its surface expression and subsequent T-cell suppression. Researchers emphasize that this approach is more durable than antibody-mediated PD-L1 blockade, as it eliminates the protein rather than just masking it.
Rational design of molecular glues has been challenging due to their unique mechanism. Most drugs are optimized to bind a single protein, but glues must stabilize a ternary complex between an E3 ligase and a target protein. Advances in cryo-EM and computational modeling now allow researchers to visualize and predict these interactions, accelerating the development of novel degraders. Machine learning algorithms trained on known glue-ligase-target triads are identifying new druggable interfaces, expanding the universe of proteins that can be pharmacologically eliminated.
The clinical success of immunomodulatory imide drugs (IMiDs) like lenalidomide proved that molecular glues could be both safe and effective. Newer compounds, such as PVTX-405, are being engineered for greater specificity, minimizing off-target degradation. By fine-tuning the affinity between the glue, ligase, and target, scientists aim to create degraders that act with surgical precision, avoiding the hematologic toxicities seen with earlier agents.
As the field matures, molecular glues are transitioning from fortuitous discoveries to deliberately engineered therapeutics. The next generation of these compounds will target previously “undruggable” oncoproteins, offering hope for cancers that have eluded conventional therapies.
Mechanistic Mastery: How PVTX-405 Rewires Immune Evasion
PVTX-405 operates at the nexus of protein degradation and immune modulation. Its primary target, PD-L1, is a critical checkpoint protein that tumors overexpress to deactivate cytotoxic T-cells. While antibodies like atezolizumab block PD-L1’s interaction with PD-1, PVTX-405 goes further—ensuring PD-L1 never reaches the cell surface in the first place.
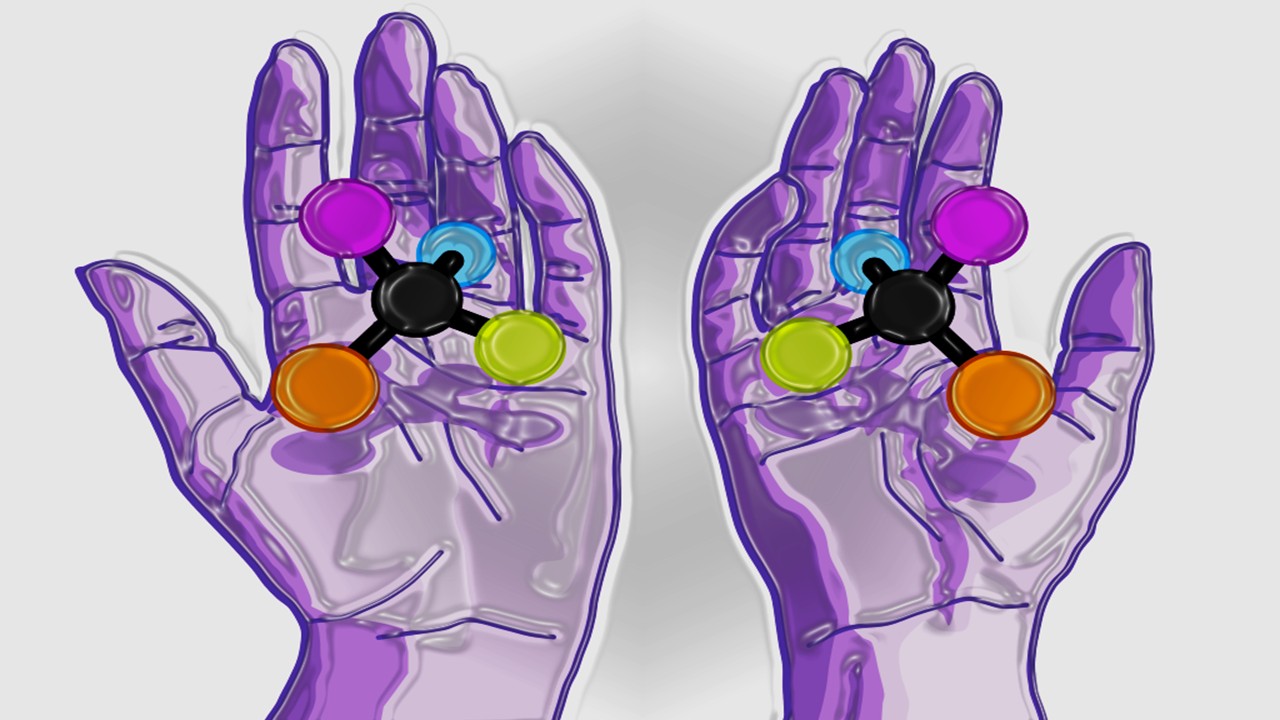
The drug’s mechanism hinges on cereblon, an E3 ubiquitin ligase that normally regulates neural development. PVTX-405 acts as a molecular matchmaker, binding cereblon and PD-L1 simultaneously, inducing a neo-interaction that flags PD-L1 for proteasomal degradation. Structural studies reveal that the glue induces a conformational change in cereblon, creating a novel binding pocket that accommodates PD-L1’s cytoplasmic domain. This ternary complex is then polyubiquitinated, marking PD-L1 for destruction.
Unlike transcriptional inhibitors that indirectly reduce PD-L1 levels, PVTX-405 acts post-translationally, achieving rapid and complete protein clearance. This is crucial in the dynamic tumor microenvironment, where PD-L1 expression can fluctuate in response to inflammatory signals. By continuously degrading PD-L1, the drug prevents tumor cells from adapting to immune pressure, a common failure mode of checkpoint inhibitors.
The effects extend beyond PD-L1 suppression. Proteomic analyses show that PVTX-405 also destabilizes other immunosuppressive factors, such as CD47 and B7-H3, which collaborate with PD-L1 to establish an immune-excluded tumor niche. This polypharmacology enhances T-cell infiltration and activation, converting “cold” tumors into “hot” ones susceptible to immune clearance. Researchers suggest that this broad-spectrum immune remodeling could overcome resistance to single-agent checkpoint blockade.
Preclinical models demonstrate that PVTX-405 synergizes with adoptive cell therapies, enhancing the persistence and cytotoxicity of infused T-cells. In melanoma and NSCLC xenografts, the combination led to complete regressions, with no evidence of immune-related toxicity. The drug’s ability to selectively degrade immunosuppressive proteins in tumor cells—while sparing healthy tissues—positions it as a cornerstone of next-generation immunotherapy regimens.
Beyond PD-L1: Expanding the Universe of Degradable Targets
While PD-L1 degradation is a compelling application, molecular glues have far broader potential. The modularity of the ubiquitin-proteasome system means that, in theory, any protein with a solvent-exposed degron motif can be targeted for elimination. Recent work has identified glues that degrade transcription factors, kinases, and even previously “undruggable” scaffold proteins.
One promising avenue is the degradation of STAT3, a transcription factor central to tumor survival and immune evasion. Traditional inhibitors struggle to disrupt STAT3’s SH2 domain-mediated dimerization, but a novel glue compound forces its interaction with the E3 ligase VHL, leading to rapid degradation. In triple-negative breast cancer models, this approach suppressed tumor growth more effectively than small-molecule inhibitors, with no compensatory JAK-STAT pathway activation.
Another frontier is targeting oncogenic fusion proteins, such as BCR-ABL in CML. Resistance mutations often render kinase inhibitors ineffective, but a molecular glue that recruits BCR-ABL to the CRBN ligase could bypass this issue. Early-stage glues are showing activity against T315I-mutant BCR-ABL, a variant resistant to all approved TKIs, suggesting a path forward for refractory patients.
Non-protein targets are also being explored. A recently discovered glue induces the degradation of the lncRNA MALAT1 by tethering it to the exosome complex. Since MALAT1 promotes metastasis in multiple cancers, its selective removal could inhibit tumor spread without genomic editing. This expands the scope of degraders beyond the proteome, opening possibilities for RNA-targeted oncology.
The challenge lies in achieving absolute specificity. Many E3 ligases, like cereblon, have endogenous substrates critical for normal physiology. Off-target degradation of these proteins can lead to toxicity, as seen with IMiD-induced teratogenicity. New glues are being designed to exploit tissue-specific E3 ligases or engineered synthetic ligases that have no natural partners, minimizing collateral damage.
As the repertoire of degradable targets grows, molecular glues could become a universal tool for precision oncology. The key will be balancing potency with selectivity, ensuring that only the intended proteins are marked for destruction.
Delivery and Pharmacokinetics: Engineering Glues for Clinical Success
The therapeutic potential of molecular glues hinges on their ability to reach target cells in sufficient concentrations. Unlike antibodies, which have predictable pharmacokinetics, small-molecule degraders must overcome membrane permeability, metabolic stability, and tissue distribution challenges. PVTX-405’s design incorporates several innovations to address these hurdles.
The compound’s core structure is derived from phthalimide, like its IMiD predecessors, but with strategic modifications to enhance solubility and half-life. A polyethylene glycol (PEG) moiety improves aqueous stability, while a masked tertiary amine prevents premature hepatic clearance. These tweaks allow for oral bioavailability, a significant advantage over biologic checkpoint inhibitors that require intravenous infusion.
Tumor penetration is another critical factor. Many targeted therapies fail in solid tumors due to poor extravasation and dense stromal barriers. PVTX-405’s low molecular weight (<500 Da) enables passive diffusion into poorly vascularized regions, where immunosuppressive proteins like PD-L1 are often most abundant. Imaging studies in glioblastoma models show uniform distribution across the blood-brain barrier, a rare feat for cancer drugs.
Metabolic resistance is a common issue with small-molecule glues. Cytochrome P450 enzymes can rapidly inactivate thalidomide analogs, necessitating high doses. PVTX-405 incorporates fluorine atoms at vulnerable positions, blocking oxidative metabolism without compromising E3 ligase engagement. This extends its half-life, allowing for once-daily dosing in preclinical species.
The drug’s pharmacokinetic profile is further optimized by avoiding P-glycoprotein (P-gp) efflux, a mechanism that pumps many hydrophobic compounds out of cells. By introducing a strategically placed hydroxyl group, the designers reduced P-gp recognition while maintaining cereblon binding. This ensures sustained intracellular concentrations, critical for continuous target degradation.
Clinical formulations are exploring nanoparticle encapsulation to enhance lymphatic delivery, important for hematologic malignancies. Early data suggest that liposomal PVTX-405 accumulates preferentially in lymph nodes, where it degrades PD-L1 on dendritic cells, enhancing antigen presentation. Such delivery innovations could tailor the drug for both solid and liquid tumors.
Safety and Resistance: Navigating the Challenges of Targeted Degradation
The potency of molecular glues raises legitimate safety concerns. Indiscriminate protein degradation could disrupt homeostasis, leading to unforeseen toxicities. PVTX-405’s development has focused on minimizing off-target effects while maximizing tumor-selective activity.
Cereblon’s endogenous substrates, such as SALL4 and IKZF1, are essential for embryonic development and hematopoiesis. Degradation of these proteins underlies the teratogenicity and myelosuppression seen with IMiDs. PVTX-405’s chemical modifications subtly alter cereblon’s binding interface, shifting its preference toward PD-L1 and away from developmental factors. In primate studies, the drug showed no evidence of embryonic toxicity at therapeutic doses, a promising sign for clinical use.
Another risk is paradoxical immune activation. By removing multiple checkpoint proteins, PVTX-405 could theoretically trigger cytokine storms or autoimmune reactions. However, its localized action within tumor cells appears to spare systemic immunity. Researchers note that the drug’s effects are context-dependent, requiring the inflammatory milieu of the tumor microenvironment to fully unleash T-cell responses.
Resistance to degraders is inevitable, but early insights suggest multiple counterstrategies. Some tumors downregulate cereblon to evade PVTX-405; combining it with cereblon-stabilizing agents may prevent this. Others upregulate deubiquitinases (DUBs) that remove ubiquitin chains before proteasomal recognition. Small-molecule DUB inhibitors are being tested as adjuvants to prolong target degradation.
An unexpected advantage is that resistance mutations in the target protein often destabilize it further, making degradation even easier. In contrast to kinase inhibitors, where mutations restore enzymatic activity, PD-L1 mutants that evade PVTX-405 binding tend to misfold and are eliminated by quality-control pathways. This creates a therapeutic “sweet spot” where resistance mechanisms backfire.
Long-term safety monitoring will be essential as PVTX-405 enters clinical trials. However, its precision engineering and mechanistic advantages position it as a potentially safer alternative to broad-acting immunotherapies.
Clinical Horizons: PVTX-405 in the Immunotherapy Landscape
PVTX-405 is poised to enter phase I trials for advanced solid tumors, with a focus on PD-L1-high malignancies like NSCLC and urothelial carcinoma. Its unique mechanism has attracted interest as both a monotherapy and a backbone for combination regimens.
The first-in-human study will explore escalating doses to establish the optimal balance between PD-L1 degradation and immune activation. Pharmacodynamic endpoints include tumor biopsy analyses of PD-L1 protein levels and T-cell infiltration, providing early proof of mechanism. Researchers anticipate that maximal degradation may not require maximal dosing, given the catalytic nature of ubiquitination.
Combination strategies are already being planned. Preclinical data suggest synergy with CDK4/6 inhibitors, which enhance tumor antigen presentation, and with STING agonists, which amplify innate immune sensing. A particularly intriguing avenue is pairing PVTX-405 with TCR-engineered T-cells, where degraded PD-L1 could prevent exhaustion of the infused cells.
Pediatric applications are also under exploration. Unlike checkpoint inhibitors, which have limited efficacy in children, PVTX-405’s ability to degrade B7-H3—a key immune evasion protein in pediatric sarcomas and neuroblastoma—could fill an unmet need. Early access programs are being designed for refractory childhood cancers with high B7-H3 expression.
The drug’s oral bioavailability could revolutionize immunotherapy access, eliminating the need for infusion centers. This is especially relevant in low-resource settings, where cold-chain storage of biologics is impractical. If successful, PVTX-405 may set a new standard for convenient, targeted immunotherapy.
As the trial data mature, PVTX-405 could redefine first-line treatment for multiple cancers. Its potential to convert immunologically “cold” tumors into responsive ones addresses a major limitation of current therapies, offering hope for historically resistant malignancies.
Beyond Cancer: The Broad Therapeutic Potential of Molecular Glues
While oncology is the immediate focus, molecular glue degraders have far-reaching applications. The same principles enabling PVTX-405 to dismantle cancer defenses could be applied to autoimmune diseases, viral infections, and neurodegenerative disorders.
In lupus, where aberrant plasma cells produce pathogenic autoantibodies, a cereblon-based glue is being developed to degrade IRF4, a transcription factor essential for plasma cell survival. Early models show selective depletion of autoreactive B-cells without broad immunosuppression, a significant improvement over current therapies.
Antiviral applications are equally promising. A glue targeting the HIV accessory protein Vif, which protects the virus from APOBEC-mediated degradation, could force viral clearance from latent reservoirs. Similarly, glues that degrade SARS-CoV-2’s NSP1 protein, which suppresses host translation, might provide broad-spectrum coronavirus protection.
Neurodegenerative diseases characterized by toxic protein aggregates, such as tauopathies and synucleinopathies, could benefit from glues that enhance clearance of misfolded proteins. A tau-directed glue recruiting the E3 ligase CHIP is in preclinical testing for Alzheimer’s, with preliminary evidence of reduced neurofibrillary tangles.
The modularity of the approach suggests that, with the right ligase-glue pair, nearly any pathogenic protein could be targeted. As the toolbox of E3 ligases expands—including engineered ligases with artificial substrate specificity—the therapeutic possibilities will grow exponentially.
A New Era of Pharmacological Precision
Molecular glue degraders like PVTX-405 represent a quantum leap in targeted therapy. By co-opting the cell’s own degradation machinery, they achieve a level of precision that eludes traditional inhibitors, turning undruggable targets into therapeutic vulnerabilities.
The implications for cancer immunotherapy are profound. Instead of merely blocking immune checkpoints, these compounds erase them entirely, offering a more durable and potentially safer approach. As PVTX-405 advances through clinical trials, it may herald a new class of drugs that combine the specificity of biologics with the convenience of small molecules.
Beyond oncology, the glue degrader platform promises to revolutionize treatment across therapeutic areas. The next decade will likely see an explosion of these agents, each designed to eliminate a specific disease-causing protein with exquisite selectivity.
In the grand narrative of drug discovery, molecular glues mark a shift from inhibition to elimination—from modulating biology to rewriting it. As this technology matures, it may well become the cornerstone of 21st-century medicine.
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES

Subscribe
to get our
LATEST NEWS
Related Posts

Medicinal Chemistry & Pharmacology
Polarity Alchemy: Strategic Charge Manipulation in Contemporary Drug Design
The future promises tunable therapies with polarity adjustable by light, magnetic fields, or bioorthogonal triggers.

Medicinal Chemistry & Pharmacology
Metabolic Saboteurs: Precision Drug Design Against Pathological Pathways
The next frontier in precision medicine lies in drugs that surgically disrupt disease-specific metabolic pathways and recalcitrant enzymes.
Read More Articles
Optimizing Freight Consolidation: Unlocking Efficiency in Multi-Modal Transport for Pharmaceutical Supply Chains
By employing multi-modal systems, where goods are transferred seamlessly between different transportation methods, stakeholders in the pharmaceutical industry can unlock substantial improvements in both efficiency and cost management
Chemical Gale: How Wind Energy is Reshaping Industrial Manufacturing
The integration of wind energy into chemical manufacturing constitutes a fundamental reimagining of process chemistry.