As we progress through an era of biomedical innovation, the use of nanoparticles has emerged as a significant tool in drug delivery and imaging technologies. These ultra-small, versatile particles have captured the attention of scientists for their potential to revolutionize therapeutic and diagnostic applications. However, despite the increasing body of research, the translation of nanoparticle systems from the laboratory to clinical practice remains limited. This article explores the challenges, the advances in nanoparticle drug delivery, and the steps that are necessary to enhance the clinical applicability of these promising technologies.
From Promise to Practice: Challenges in Nanoparticle Drug Delivery
The allure of nanoparticle-based drug delivery lies in its capacity to enhance the effectiveness of therapeutic agents. By increasing circulation time, improving disease targeting, and providing controlled payload release, these systems offer a high degree of sophistication. Yet, despite this, few nanoparticle formulations have crossed the chasm from the bench to bedside application. The scientific community is increasingly aware of this gap, necessitating a thorough re-evaluation of design strategies and testing protocols to improve clinical success rates.
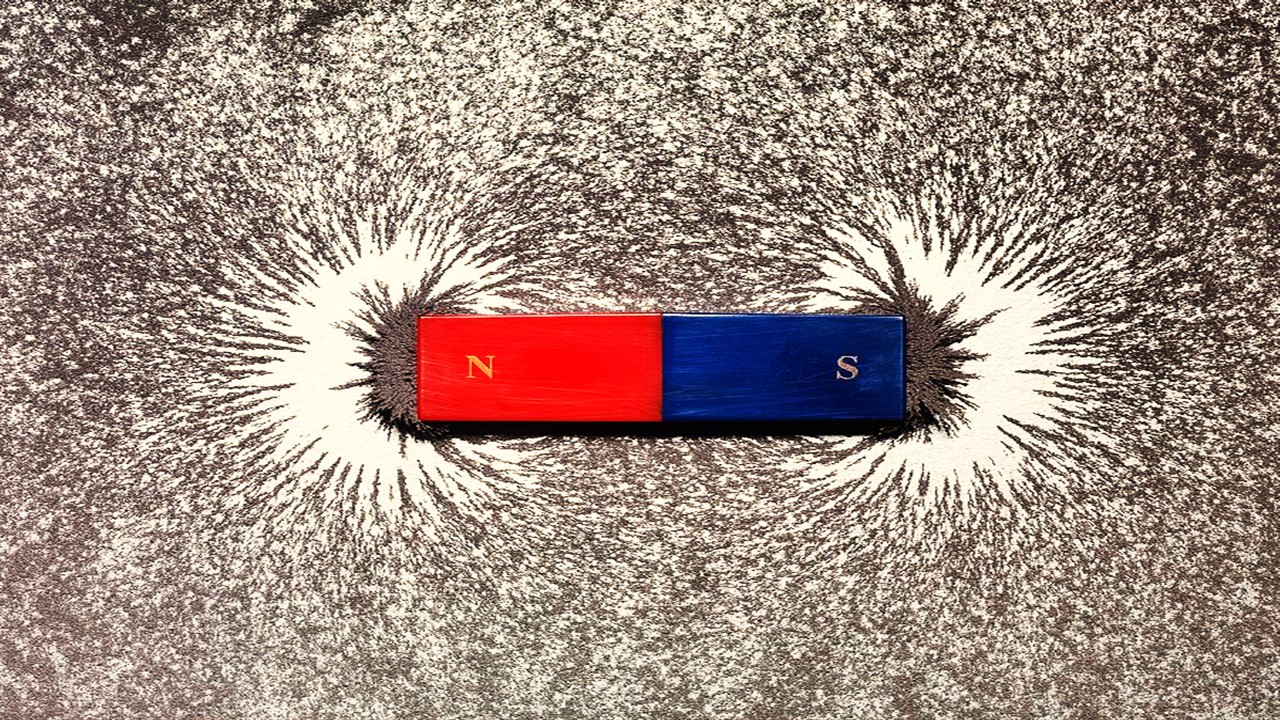
Nanoparticles can be engineered to address various demands within the body. Their surfaces are often modified with polyethylene glycol (PEG), tumor-targeting peptides, or environmentally responsive linkers. These modifications are aimed at extending their circulation time, enabling targeted delivery to diseased tissues, and enhancing retention at the intended site. However, the true challenge emerges at the nano–bio interface—where nanoparticles interact with the body’s biological milieu, particularly the immune system. This interface is primarily mediated by opsonization, a process that coats nanoparticles with proteins, forming what is known as the protein corona. The protein corona plays a pivotal role in determining the biological fate of these particles, influencing their clearance, uptake, and distribution. Unfortunately, while nanoparticle characterization and fabrication methods have evolved significantly, the understanding of how these particles interact with the immune system has lagged, potentially undermining their clinical effectiveness.
Nanoparticles in the Clinical Landscape
Despite the challenges, several nanoparticle formulations have achieved FDA approval or are undergoing clinical trials for specific therapeutic applications. These formulations typically use compounds such as PEG, methoxy-PEG (mPEG), or poly(lactic-co-glycolic acid) (PLGA) to extend their circulation time and improve their targeting capabilities.
For instance, Mircera, formulated with methoxypolyeletheneglycol-epoetin beta, has been approved for the treatment of anemia associated with chronic renal failure. Similarly, PegIntron, a pegylated form of interferon alpha-2b, is FDA-approved for managing HIV-related inflammation. These examples represent just a few of the growing number of nanoparticles being used to address a wide range of diseases, from cancer and viral infections to chronic inflammation and hematologic conditions.
However, clinical translation is not always straightforward. The protein corona, which rapidly forms on the nanoparticle surface after administration, often masks the particle’s intended design, shifting its biological behavior and response. This interaction is critical because it alters how nanoparticles are recognized and processed by the immune system, particularly through macrophages and dendritic cells. Proteins such as albumin or opsonins—including fibrinogen and immunoglobulins—bind to the nanoparticle surface, tagging it for phagocytosis. These processes, controlled by the body’s mononuclear phagocyte system (MPS), dictate the clearance of nanoparticles and can thwart efforts to prolong their circulation time.
Interestingly, some nanoparticle formulations, such as Caelyx and Doxil, which encapsulate doxorubicin within pegylated liposomes, have shown promise in extending the drug’s half-life and improving its distribution in cancer treatment. However, the formation of the protein corona remains a double-edged sword. While it can reduce the burst release of the drug, as seen with Abraxane, it can also destabilize the nanoparticle structure, leading to premature drug release, as observed with formulations like Doxova.
The Nano–Bio Interface: Navigating the Protein Corona
One of the most fascinating, yet challenging, aspects of nanoparticle drug delivery lies in the formation of the protein corona. Once a nanoparticle enters the bloodstream, it is immediately coated with proteins. This protein layer can obscure the synthetic identity of the nanoparticle, replacing it with a biological one that the immune system reacts to. The composition of the corona is not static; it changes based on the biological environment and the body’s immune response. This dynamic interaction influences whether the nanoparticle will be cleared by macrophages or remain in circulation long enough to deliver its therapeutic payload.
Hydrophobic nanoparticles tend to bind more strongly to apolipoproteins, while hydrophilic particles, which attract proteins like fibrinogen and albumin, display a lower rate of clearance. Moreover, nanoparticles that are bound by hydrophobic proteins tend to be quickly flagged for clearance by the immune system, while those with hydrophilic coatings can evade detection for longer periods, reducing complement activation and immune response.
PEGylation, a common surface modification technique, has been shown to increase nanoparticle circulation time. However, this approach can also enhance the nanoparticle’s interaction with immune-competent proteins, making it more susceptible to detection and clearance. On the other hand, coatings with pluronic F127 or the use of zwitterionic particles have been associated with decreased serum protein adsorption, increasing nanoparticle dispersion and reducing clearance rates.
Mechanisms of Immune Clearance: Overcoming the MPS
The interaction between nanoparticles and the immune system, particularly the MPS, is a critical determinant of nanoparticle fate in the body. The MPS, responsible for deploying macrophages and monocytes, is also the key player in the clearance of nanoparticles. Several strategies have been explored to overcome the MPS and extend the therapeutic window of nanoparticle systems. These include passive strategies, such as increasing circulation half-life, and active strategies, such as escaping macrophage uptake.
Upon encountering a nanoparticle, macrophages begin the process of clearance through phagocytosis or pinocytosis. Phagocytosis, which is size-dependent, is the primary mechanism of clearance for nanoparticles between 50 and 200 nm. Nanoparticles are engulfed in a multi-step process that involves recognition, engulfment, and degradation. However, if the particle is small enough or its surface chemistry sufficiently altered, it may evade complete engulfment, allowing it to remain in circulation.
Research into strategies that can saturate or temporarily overwhelm macrophage activity shows potential. For instance, injecting nanoparticles composed of phosphatidyl-choline and cholesterol (PC: Chol) into the liver can saturate macrophages, allowing subsequent therapeutic nanoparticles to evade immediate clearance. While this strategy raises intriguing possibilities, the safety of such approaches remains a significant concern, particularly in clinical settings.
The Final Frontier: Optimizing Nanoparticle Design for Immune Evasion and Therapeutic Success
Surface chemistry, particularly the charge and hydrophobicity of nanoparticles, further dictates their interaction with biological systems. Positively charged particles are more prone to rapid clearance through opsonization, while hydrophilic or neutral particles exhibit extended circulation times due to reduced interactions with immune cells. The development of a protein corona on the nanoparticle surface adds another layer of complexity, influencing immune recognition and clearance. Nanoparticles with hydrophobic surfaces are more likely to trigger danger signals and rapid clearance, whereas hydrophilic surfaces, such as PEGylated coatings, help mitigate these immune responses and prolong circulation.
Despite significant progress in nanoparticle design, challenges remain in fully understanding and controlling their interactions with the immune system. The dual roles of macrophages in both removing nanoparticles and priming immune responses highlight the complexity of achieving therapeutic success. As researchers continue to explore the nuances of nanoparticle biology, optimizing the interplay between size, shape, surface chemistry, and immune evasion will be key to advancing these technologies from the bench to the bedside, realizing their full potential in drug delivery and biomedical applications.
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES
Subscribe
to get our
LATEST NEWS
Related Posts

Medicinal Chemistry & Pharmacology
Aerogel Pharmaceutics Reimagined: How Chitosan-Based Aerogels and Hybrid Computational Models Are Reshaping Nasal Drug Delivery Systems
Simulating with precision and formulating with insight, the future of pharmacology becomes not just predictive but programmable, one cell at a time.

Medicinal Chemistry & Pharmacology
Coprocessed for Compression: Reengineering Metformin Hydrochloride with Hydroxypropyl Cellulose via Coprecipitation for Direct Compression Enhancement
In manufacturing, minimizing granulation lines, drying tunnels, and multiple milling stages reduces equipment costs, process footprint, and energy consumption.

Medicinal Chemistry & Pharmacology
Decoding Molecular Libraries: Error-Resilient Sequencing Analysis and Multidimensional Pattern Recognition
tagFinder exemplifies the convergence of computational innovation and chemical biology, offering a robust framework to navigate the complexities of DNA-encoded science
Read More Articles
Magnetic Nanoengineering: Overcoming Biological Variability and Enhancing Therapeutic Precision
The future of nanomedicine lies in harmonizing precision, accessibility, and ecological responsibility, ushering in an era where therapies are tailored to individual biological landscapes.
Trials, Triumphs, and Trials Ahead: Navigating the Landscape of Randomized Controlled Trials in Artificial Intelligence-Driven Healthcare
The adoption of artificial intelligence in clinical practice has prompted a surge in randomized controlled trials, highlighting a balance of enthusiasm and prudence.
Illuminating the Dark Genome: Uncharted Frontiers in Therapeutic Discovery
The dark genome is not a biological void but a frontier awaiting illumination.