The Evolution of Drug Discovery
The landscape of drug discovery has always been a meticulous and high-stakes endeavor. Traditionally, drug development began with screening pharmacological agents for desirable activity, followed by stringent preclinical testing to assess safety, efficacy, and toxicity. After this, the process moves through human clinical trials to validate these findings and eventually, a drug application is submitted to regulatory authorities for approval. While this process seems linear, it is riddled with significant challenges—particularly in preclinical models where most drugs fail to make the leap from laboratory testing to successful human trials.
Traditional preclinical models have largely relied on in vitro and in vivo methods, primarily utilizing human cell cultures and non-human animal models, respectively. These models have long been central to the characterization of drug candidates’ biological properties, such as pharmacodynamics (PD), pharmacokinetics (PK), and toxicological profiles. However, despite their widespread use, these models often fall short in accurately predicting how a drug will perform in humans.
The Preclinical Bottleneck: Limitations of Current Models
In drug discovery, preclinical models play a crucial role in evaluating a compound’s safety and efficacy before advancing to human clinical trials. For decades, in vitro cell cultures and small animal models like rodents have served as the backbone of this phase. Researchers can screen numerous drug candidates rapidly, hoping to identify promising leads. However, the reliance on these traditional models has significant shortcomings that have been exposed over time.
A major limitation arises from the biological differences between small animal models and humans. Key anatomical, metabolic, and immunological disparities often result in a failure to accurately predict human-specific responses. Small animals, particularly rodents, have fundamental differences in organ structure, tissue regeneration, and drug metabolism. Even large animals like pigs and non-human primates, while offering closer physiological similarities to humans, still do not perfectly replicate human biology. As a consequence, a significant proportion of drugs that perform well in these preclinical models fail to translate into successful human therapies.
Additionally, while high-throughput screening (HTS) using in vitro models has provided a valuable platform for identifying potential drug leads, these assays are typically conducted in two-dimensional (2D) cell cultures that do not fully represent the complexity of human tissues. Monogenic diseases and well-characterized genetic disorders, such as spinal muscular atrophy or some cancers, are more amenable to these models. However, the predictive value of these systems is low, with fewer than 10% of leads from in vitro studies progressing to successful clinical trials. This disconnect between simplistic preclinical models and the intricacies of human disease underscores the urgent need for more sophisticated and representative systems.
Bridging the Gap: Emerging Models and Technological Advancements
The inefficacies of traditional preclinical models have triggered a new wave of innovation in drug discovery, with researchers turning to advanced biological and engineering tools to develop more representative human tissue models. These modern approaches aim to enhance the predictive accuracy of preclinical studies and provide new platforms for drug discovery that reflect human biology more closely.
One of the most significant advances is the development of three-dimensional (3D) in vitro models. Unlike their 2D counterparts, 3D models allow for the creation of vascularized tissue structures that better mimic the integrated dynamics of human organs. Tissue engineering and microfabrication techniques enable researchers to cultivate complex tissues in the laboratory, providing an experimental system that replicates the spatial and functional organization of human tissues. These 3D models allow for a more nuanced investigation of drug effects on multicellular environments, offering a more accurate representation of human physiology.
Stem cell-derived human cells have also gained prominence as an indispensable tool in the development of these advanced models. The ability to derive human tissues from stem cells has opened the door for creating disease-relevant in vitro systems. Combined with advances in genetic tools, researchers can now generate human tissue models with greater precision, incorporating disease-specific mutations and other molecular alterations that drive disease progression.
This shift towards human tissue models in preclinical studies is not only helping to bridge the gap between in vitro discovery and in vivo validation but is also providing new insights into human disease mechanisms. For instance, using patient-derived stem cells to create tissue-specific models allows researchers to study diseases like cancer or neurodegenerative disorders in the context of the human microenvironment. The hope is that these models will improve drug efficacy predictions while also reducing the likelihood of adverse events when the drugs enter human trials.
Revolutionizing Preclinical Testing with Human Models
Traditional animal models have offered limited utility in predicting drug efficacy, particularly in conditions that are distinctly human, such as metabolic disorders or complex neurodegenerative diseases. Even large animal models, while offering closer physiological analogs, introduce high costs, extended timelines, and ethical concerns. As such, researchers are increasingly turning to human-based preclinical models.
Human organ-on-chip technologies represent a transformative step forward in drug discovery. These microphysiological systems are designed to replicate key features of human organs at the cellular and molecular levels. For example, liver-on-chip and lung-on-chip systems provide a way to test drug metabolism and toxicity under conditions that closely resemble human physiology. These models hold immense promise in identifying drug leads that are not only more effective but also safer by offering more reliable predictions of how a drug will behave in human systems.
Furthermore, organoids—miniaturized, 3D versions of organs grown from stem cells—are another exciting development in the field. These models provide a way to study organ-specific diseases and test drug responses in a more physiologically relevant environment than standard cell cultures. Organoids are especially useful for modeling diseases with complex tissue architecture, such as cancer or liver disease. By integrating human-derived cells into these systems, scientists can study patient-specific responses to drugs, advancing the personalized medicine paradigm.
Reimagining Drug Discovery: Integrating Modern Preclinical Models
While these advanced human-based preclinical models offer great promise, they are best viewed as complementary tools that augment, rather than replace, traditional preclinical approaches. The future of drug discovery will likely involve a hybrid strategy, integrating both human-based models and in vivo animal models to create a comprehensive and predictive platform for testing drug candidates.
Incorporating these new models into drug discovery pipelines could substantially improve the translation of preclinical findings to clinical success. For example, combining in vitro human organoids with in vivo validation in large animal models offers a powerful dual approach. The organoids provide a human-specific platform for early-stage discovery, while large animal models allow for more rigorous testing of pharmacokinetics and toxicity under conditions that resemble human metabolism and immune responses.
These advances in preclinical testing are also helping to unlock new avenues of drug discovery that were previously inaccessible. Improved understanding of complex disease mechanisms, such as cancer metastasis or neurodegenerative disease progression, will allow researchers to target previously undruggable pathways. The development of more sophisticated models enables screening of combination therapies, opening new doors in oncology, immunotherapy, and regenerative medicine.
Paving the Way for Predictive Precision
The evolution from traditional to modern lead discovery represents a pivotal moment in drug development. As the pharmaceutical industry faces increasing challenges in bringing new therapeutics to market, there is a growing recognition that traditional preclinical models, while valuable, have fundamental limitations. The shift towards human-based, engineered models reflects an ongoing effort to overcome these barriers and make the drug discovery process more predictive, efficient, and successful.
By integrating human tissue models, organ-on-chip systems, and advances in stem cell biology, researchers are forging a new path for drug discovery—one where the gap between preclinical testing and human clinical trials is narrower, and the promise of personalized medicine comes ever closer to fruition. This reimagined approach is not only poised to enhance the success of drug candidates but is also revolutionizing our understanding of human disease. In doing so, it marks a critical step forward in modern medicine, with the potential to shape the future of therapeutic innovation.
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES
Subscribe
to get our
LATEST NEWS
Related Posts

Drug Discovery Biology
Proteolytic Rewriting: Engineering Controlled Absence of Pathogenic Protein Persistence
Targeted protein degradation transforms drug therapy by engineering the cellular machinery to erase, rather than merely inhibit, pathogenic proteins.

Drug Discovery Biology
Open Nucleotides: Grant-Driven Infrastructure for Equitable mRNA Vaccine Manufacturing
By developing accessible cap analogs and RNA raw materials, Hongene Biotech, guided by David Butler’s expertise in nucleotide chemistry and supported by the Gates Foundation, is reshaping the molecular infrastructure that underpins global mRNA vaccine equity.
Drug Discovery Biology
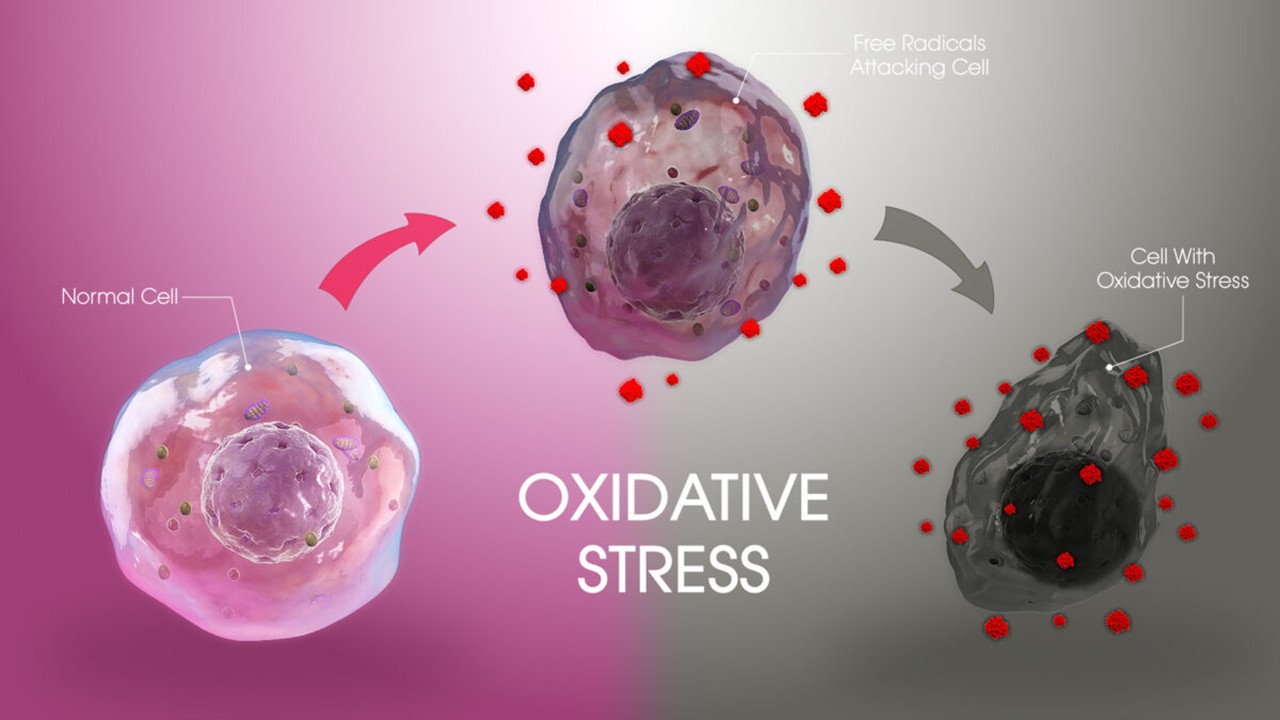
Redox Messengers: How Endogenous Gasotransmitters Rewire Vascular Biology to Resist Age-Driven Oxidative Stress
Gasotransmitters provide a biologically sophisticated means of counteracting age-related oxidative stress and preserving vascular resilience.
Drug Discovery Biology
Aptamer Signal Dynamics: Engineering Nucleic Acid Recognition Systems for High-Fidelity, Multi-Modal Biosensing
Aptamers redefine biosensing by pairing programmable molecular recognition with versatile transduction strategies capable of detecting clinically relevant biomarkers with exceptional fidelity.
Read More Articles
Spatial Collapse: Pharmacologic Degradation of PDEδ to Disrupt Oncogenic KRAS Membrane Localization
PDEδ degradation disrupts KRAS membrane localization to collapse oncogenic signaling through spatial pharmacology rather than direct enzymatic inhibition.
Neumedics’ Integrated Innovation Model: Dr. Mark Nelson on Translating Drug Discovery into API Synthesis
Dr. Mark Nelson of Neumedics outlines how integrating medicinal chemistry with scalable API synthesis from the earliest design stages defines the next evolution of pharmaceutical development.
Zentalis Pharmaceuticals’ Clinical Strategy Architecture: Dr. Stalder on Data Foresight and Oncology Execution
Dr. Joseph Stalder of Zentalis Pharmaceuticals examines how predictive data integration and disciplined program governance are redefining the future of late-stage oncology development.
Exelixis Clinical Bioanalysis Leadership, Translational DMPK Craft, and the Kirkovsky Playbook
Senior Director Dr. Leo Kirkovsky brings a rare cross-modality perspective—spanning physical organic chemistry, clinical assay leadership, and ADC bioanalysis—to show how ADME mastery becomes the decision engine that turns complex drug systems into scalable oncology development programs.
Policy Ignition: How Institutional Experiments Become Durable Global Evidence for Pharmaceutical Access
Global pharmaceutical access improves when IP, payment, and real-world evidence systems are engineered as interoperable feedback loops rather than isolated reforms.
Sepsis Shadow: Machine-Learning Risk Mapping for Stroke Patients with Bloodstream Infection
Regularized models like LASSO can identify an interpretable risk signature for stroke patients with bloodstream infection, enabling targeted, physiology-aligned clinical management.







