Alzheimer’s Disease is the leading cause of dementia worldwide, yet few treatment options are available to most people in the world, if any. Of people aged 65 or older, 11.63% have Alzheimer’s, with 1 in 3 seniors in America dying with it. As the average lifespan of humans worldwide increases, the prevalence of Alzheimer’s is sure to follow the same trend in our aging populations. As such, the urgency for new Alzheimer’s treatments remains great.
The most common features of Alzheimer’s Disease involve memory failure, as well as other behavioural changes such as poor judgment, language disturbance, agitation, and can also manifest with more severe symptoms such as Parkinsonian features, incontinence, and mutism. Death can come about as a result of these symptoms – e.g. malnutrition, or generally increased susceptibility to secondary diseases such as pneumonia.
It should be noted that Alzheimer’s Disease is not only lethal, but is severely disabling for a significant amount of time – it can last for over a decade prior to death. As such, the burden of Alzheimer’s should not only be measured through fatalities, but also in the number of years lived with disabilities originating from the disease.
Physiology of Alzheimer’s Disease
Physiologically, the symptoms of Alzheimer’s Disease are striking. It starts with an abnormal amount of amyloid beta (Aβ) accumulating in the brain’s extracellular matrix where they form amyloid plaques. Conversely, tau proteins accumulate inside brain cells and impair function by forming tangles. Additionally, cholinergic neurons, responsible for releasing the neurotransmitter acetylcholine, show a reduction in function which decreases the overall acetylcholine available in the brain. It is uncertain whether any of these features are causative in Alzheimer’s Disease or whether they are merely symptoms, although multiple competing hypotheses exist.
As such, treatments can target a variety of these main symptoms. Current treatment options include acetylcholinesterase inhibitors which inhibit enzymes that can break down acetylcholine. The resultant increased levels of acetylcholine can delay further progress of the disease with small benefits. Glutamate, a different neurotransmitter, can reach abnormally high levels in individuals with Alzheimer’s. Treatment with NMDA antagonists can stop glutamate from stimulating brain cells to toxic levels, preventing cell death. Aside from these two classes of drugs, the only other current treatment options for Alzheimer’s are behavioural and palliative.
Amyloid Beta Related Treatments
Evidently, no treatment option has yet been developed that can significantly treat the disease. One of the most popular avenues of research has been to utilise the immune system by producing antibodies,which can target the plaque buildup from amyloid beta. Multiple candidates in this area have made progress as of late – Lecanemab, a drug which binds to a soluble form of amyloid beta, is currently in Phase III trials. Another antibody treatment that shows promise is Donamenab, which reduces both the levels of amyloid plaque and of tau protein.
Another antibody-based treatment, Aducanumab, was approved by the FDA in 2021, marketed as Aduhelm by Biogen. The approval sparked controversy as it was subject to a fast track process as it had not cleared Phase III trials yet. Regardless, Biogen presented new analyses this week which show a modest reduction in both amyloid plaque and tau protein levels. The drug has not yet received approval from the EMA, although this may remain the case until better data becomes available. Considering the backlash the FDA faced over its own approval of the drug, as well as the resignations of multiple FDA advisory committee members in response to the subsequent controversy, it is likely that regulators will remain skeptical, barring new data.
In other news in the field this week, new research on mice has demonstrated the possibility of a vaccine for Alzheimer’s Disease, published in Nature. The research originally started by using antibodies to break down truncated forms of amyloid beta protein, the form that leads to plaque formation due to their ability to clump together. These antibodies do this without interfering with normal amyloid beta proteins, which are necessary for brain function. They also show no preference for binding to amyloid plaque, as antibodies which target plaque directly have previously been linked to other adverse effects.
The antibody therapy itself has shown that it can lead to lower levels of amyloid beta plaque as well as increased neuron function. The research went one step further by engineering a protein similar to truncated amyloid beta, which can trigger the immune system to produce antibodies for the protein, prior to even developing any plaque themselves. This effectively makes the treatment a vaccination. In mice models, the vaccine was just as effective at symptom relief as the actual antibodies. Whether this can be replicated in human trials remains to be seen, although the research is no doubt indicative of developments in the area continuing unabated.
There are also other treatments which interact with the amyloid effects of Alzheimer’s Disease, besides antibodies. AstraZeneca has been trialing Saracatinib, which it had originally developed as a cancer treatment, in patients with Alzheimer’s. Saracatinib works by blocking the protein that enables beta amyloid to damage neurons. It is hoped that this will enable the therapeutic to halt neuronal degeneration and mental decline.
Tau Protein Treatments
Treatments that interact with tau proteins are also being developed. One such candidate is semorinemab, developed by AC Immune and Genentech, which is an antibody that targets the tau proteins and slows their spread throughout the brain. Findings presented earlier this year, show that the treatment slowed decline on the Alzheimer Disease Assessment Scale. However, it showed no effects on the Mini-Mental State Examination, or the Clinical Dementia Range-Sum of Boxes – all three of which are indicators of mental function. As such, more research in the area is required, with trials still ongoing.
Anti-Inflammatory Treatments
Novel treatment strategies that target other aspects of the disease are also being developed. Immunebio is currently working on Xpro1595. Xpro1595 is a Tumor Necrosis Factor (TNF) inhibitor which targets only soluble TNF. Soluble TNF is present in elevated levels in patients with Alzheimer’s, indicating a high degree of inflammation – which could be one of the main drivers of the brain damage observed. Xpro1595 has shown promising results in mice models, relieving cognitive failure and improving neuron function, among other positive results. The fact that it only binds to soluble TNF, rather than a wider range of TNF, is expected to lessen its potential for adverse effects. Its Phase II trial was planned this year.
Other treatment options are also being explored. Insulin resistance is one other effect that has a noted correlation with Alzheimer’s Disease, and a potential avenue of research. However, this area requires further exploration. Overall, the field of Alzheimer’s therapeutics is growing – and rightly so. With the burden of Alzheimer’s Disease projected to increase, and the current lack of widely accepted efficacious treatments, this is a field of pharma that is continuously budding with new developments. The wide variety of pathways that treatments can interact with present many opportunities for future research, as well as challenges in overcoming the disease.
Nick Zoukas, Former Editor, PharmaFeatures
Subscribe
to get our
LATEST NEWS
Related Posts

Chronic & Debilitating Diseases
Biochemical Topographies: Revealing Molecular Traces That Shape the Early Course of Diabetic Cardiomyopathy
Circulating biomarkers provide an essential roadmap for detecting the silent molecular progression of diabetic cardiomyopathy before it manifests as overt cardiac dysfunction.
Chronic & Debilitating Diseases
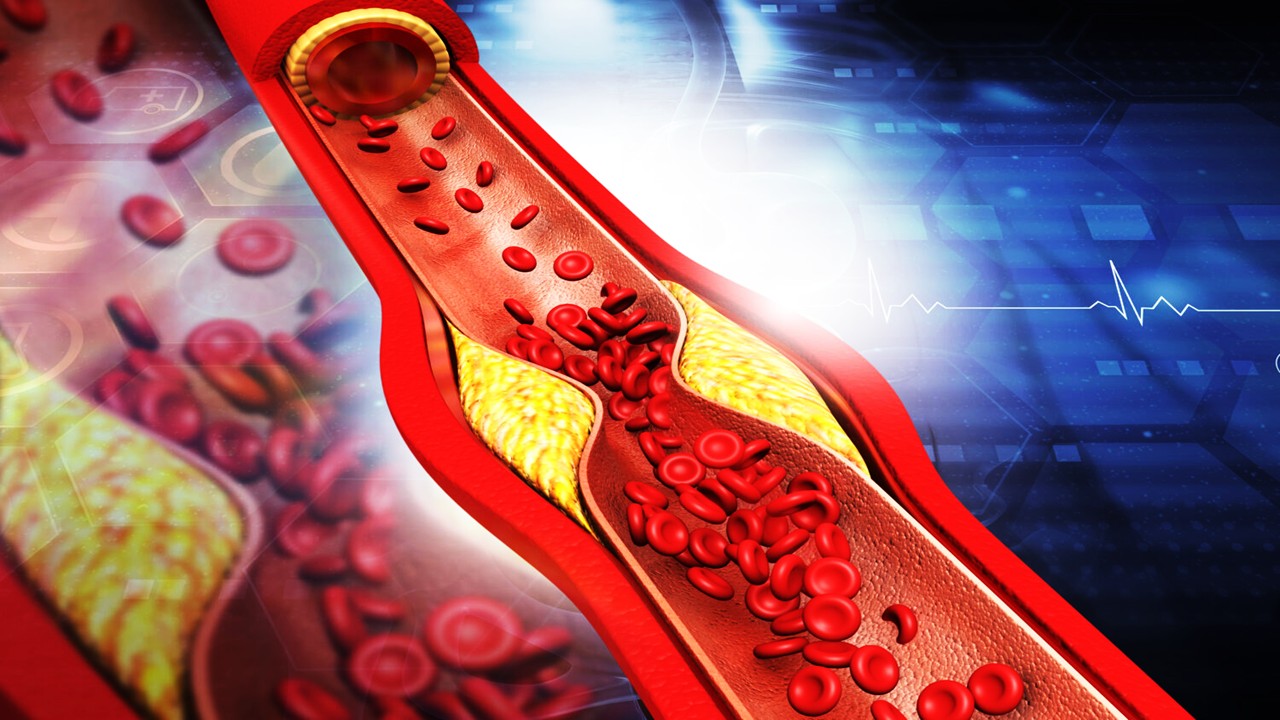
Silent Corpses, Dangerous Plaques: How Defective Cell Clearance Shapes Atherosclerosis Progression and Rupture
Failed clearance of apoptotic cells drives necrotic core expansion and inflammatory persistence, making defective efferocytosis a central determinant of atherosclerotic plaque vulnerability.
Read More Articles
Spatial Collapse: Pharmacologic Degradation of PDEδ to Disrupt Oncogenic KRAS Membrane Localization
PDEδ degradation disrupts KRAS membrane localization to collapse oncogenic signaling through spatial pharmacology rather than direct enzymatic inhibition.
Neumedics’ Integrated Innovation Model: Dr. Mark Nelson on Translating Drug Discovery into API Synthesis
Dr. Mark Nelson of Neumedics outlines how integrating medicinal chemistry with scalable API synthesis from the earliest design stages defines the next evolution of pharmaceutical development.
Zentalis Pharmaceuticals’ Clinical Strategy Architecture: Dr. Stalder on Data Foresight and Oncology Execution
Dr. Joseph Stalder of Zentalis Pharmaceuticals examines how predictive data integration and disciplined program governance are redefining the future of late-stage oncology development.
Exelixis Clinical Bioanalysis Leadership, Translational DMPK Craft, and the Kirkovsky Playbook
Senior Director Dr. Leo Kirkovsky brings a rare cross-modality perspective—spanning physical organic chemistry, clinical assay leadership, and ADC bioanalysis—to show how ADME mastery becomes the decision engine that turns complex drug systems into scalable oncology development programs.
Policy Ignition: How Institutional Experiments Become Durable Global Evidence for Pharmaceutical Access
Global pharmaceutical access improves when IP, payment, and real-world evidence systems are engineered as interoperable feedback loops rather than isolated reforms.