RNA-Based Drugs: Rewriting the Future of Infectious Disease Treatment
The emergence of RNA-based therapeutics has revolutionized the pharmaceutical landscape, offering unprecedented precision in targeting pathogens and genetic disorders. Unlike traditional small-molecule drugs, which interact with proteins, RNA therapies modulate gene expression directly, enabling interventions at the root of disease. The success of mRNA vaccines against COVID-19 demonstrated the potential of this technology, but its applications extend far beyond pandemics. Researchers are now exploring antisense oligonucleotides (ASOs), small interfering RNA (siRNA), and messenger RNA (mRNA) constructs to combat bacterial, viral, and even fungal infections with high specificity.
One of the most compelling advantages of RNA drugs is their rapid development timeline. While conventional drugs require years of optimization for target binding and pharmacokinetics, RNA sequences can be designed computationally and synthesized within weeks. This agility is critical in responding to emerging infectious threats, where traditional antibiotics and antivirals often lag behind pathogen evolution. Furthermore, RNA therapeutics can be tailored to silence virulence genes in bacteria or inhibit viral replication machinery without disrupting host cells, reducing side effects. The ability to tweak nucleotide chemistry—such as phosphorothioate backbones or 2’-O-methyl modifications—enhances stability and delivery, overcoming early limitations of rapid degradation.
Delivery remains a central challenge in RNA therapeutics. Naked RNA is vulnerable to nucleases and struggles to cross cellular membranes, necessitating advanced delivery systems. Lipid nanoparticles (LNPs), which gained fame through COVID-19 vaccines, are now being refined for broader applications, including targeting intracellular pathogens. Alternative carriers, such as peptide-based vectors or polymer nanocomplexes, are also under investigation, each offering unique advantages for tissue-specific targeting. For instance, hepatic tropism is well-established for certain LNPs, while pulmonary delivery systems are being optimized for respiratory infections. Innovations in chemical conjugation, such as GalNAc (N-acetylgalactosamine) linkages, further enhance hepatocyte uptake, opening doors for RNA drugs against hepatitis and other liver-tropic diseases.
Beyond infectious diseases, RNA therapeutics are making strides in chronic conditions and rare genetic disorders. ASOs have shown promise in treating spinal muscular atrophy and Duchenne muscular dystrophy by correcting splicing defects or blocking toxic RNA transcripts. The modularity of RNA design means that a single platform technology can be adapted for multiple diseases by simply altering the nucleotide sequence. This versatility positions RNA drugs as a universal toolkit for precision medicine, capable of addressing everything from antibiotic-resistant superbugs to neurodegenerative diseases. The next frontier involves combining RNA with gene-editing technologies like CRISPR, creating synergistic therapies that edit, silence, or replace faulty genetic material in a single treatment regimen.
Despite the excitement, hurdles remain in scaling RNA therapeutics for widespread use. Manufacturing complexities, immunogenicity risks, and cost barriers must be addressed to ensure accessibility. Early successes have validated the approach, but long-term safety and efficacy data are still accumulating. As the field matures, the integration of AI for sequence optimization and biomarker-driven patient stratification will refine therapeutic outcomes. The era of RNA medicine is just beginning, and its potential to redefine infection control and genetic therapy is unparalleled.
Oligonucleotides: Precision Tools Against Viral and Bacterial Resistance
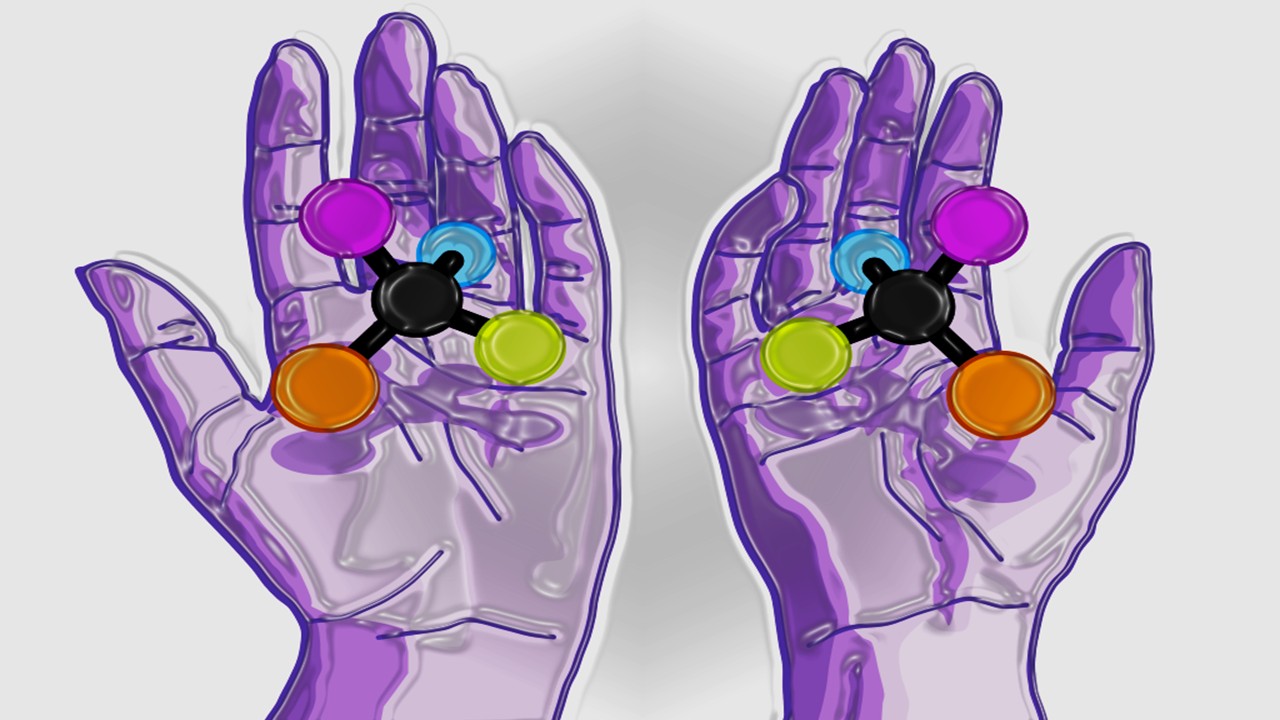
Oligonucleotide therapies, particularly antisense and siRNA agents, are emerging as powerful weapons against drug-resistant infections. These short nucleic acid strands bind complementary RNA sequences, either degrading them or blocking translation, effectively silencing critical pathogen genes. Unlike broad-spectrum antibiotics, which indiscriminately target microbial populations, oligonucleotides can be designed to attack conserved regions of viral genomes or essential bacterial transcripts, minimizing resistance development. This precision is especially valuable in treating persistent infections like HIV or tuberculosis, where conventional drugs often fail due to mutation-driven escape.
The mechanism of oligonucleotide drugs hinges on Watson-Crick base pairing, ensuring high specificity. For example, an siRNA targeting the Ebola virus’s L polymerase gene can shut down replication without affecting human cells. Similarly, ASOs designed against bacterial ribosomal RNA can inhibit protein synthesis in multidrug-resistant strains of Staphylococcus or Pseudomonas. Chemical modifications, such as locked nucleic acids (LNAs) or morpholino backbones, enhance binding affinity and nuclease resistance, prolonging therapeutic activity. These advances have transformed oligonucleotides from lab curiosities into viable clinical candidates, with several now in late-stage trials for hepatitis B and respiratory syncytial virus (RSV).
Delivery remains a bottleneck, particularly for systemic infections. While LNPs work well for hepatic targets, reaching extrahepatic tissues requires alternative strategies. Conjugation to cell-penetrating peptides (CPPs) or antibody fragments improves biodistribution, enabling oligonucleotides to cross epithelial barriers or target immune cells. Pulmonary delivery via nebulization is another promising avenue, as seen in trials for RSV and influenza. The adaptability of oligonucleotide chemistry allows researchers to fine-tune pharmacokinetics, balancing tissue accumulation with renal clearance to avoid toxicity.
The potential of oligonucleotides extends beyond single-pathogen targeting. Combinatorial approaches, where multiple ASOs or siRNAs attack different viral genes simultaneously, could preempt resistance. This strategy is being explored for HIV, where overlapping oligonucleotides might suppress viral load more durably than small-molecule antiretrovirals. Another frontier is prophylactic oligonucleotides—short-term treatments that prime the immune system to recognize and neutralize pathogens before they establish infection. Such applications could revolutionize outbreak containment, particularly in high-risk settings like hospitals or pandemic hotspots.
Despite their promise, oligonucleotide therapies face challenges in cost and scalability. Synthesis of modified nucleotides is expensive, and large-scale production must become more efficient to compete with conventional drugs. Immunostimulatory side effects, such as unintended Toll-like receptor activation, also require careful monitoring. However, as delivery technologies improve and manufacturing costs decline, oligonucleotides could become mainstream tools in the antimicrobial arsenal, offering a stopgap against the rising tide of resistance.
Polypeptide Therapeutics: Bridging Small Molecules and Biologics
Polypeptides—chains of amino acids ranging from 10 to 100 residues—occupy a unique niche between small-molecule drugs and large biologics. Their intermediate size allows for high specificity and potency while retaining synthetic tractability and tissue penetration. Antimicrobial peptides (AMPs), a subset of polypeptides, have long been studied for their ability to disrupt bacterial membranes, but recent engineering advances are expanding their utility against viruses, fungi, and even cancer. Unlike traditional antibiotics, which target specific enzymes, AMPs often act via physical membrane disruption, making resistance less likely to evolve.
The structural diversity of polypeptides enables multifunctionality. Some are designed to mimic host defense peptides, like human cathelicidin LL-37, which not only kills microbes but also modulates immune responses. Others incorporate non-natural amino acids or cyclic constraints to enhance stability against proteases. For example, teixobactin, a recently discovered cyclic peptide, shows potent activity against Gram-positive bacteria by binding lipid II, a cell wall precursor. Such innovations are revitalizing interest in peptide antibiotics, which had been sidelined due to poor pharmacokinetics in earlier generations.
Peptide therapeutics are also making waves in antiviral research. Fusion inhibitors, such as enfuvirtide for HIV, block viral entry by mimicking host cell receptors. Newer designs target conserved regions of viral glycoproteins, thwarting escape mutations. In oncology, peptide-drug conjugates (PDCs) deliver cytotoxic payloads to tumors with high precision, minimizing off-target effects. The same targeting principles are being adapted for infectious diseases, where peptides could ferry antivirals or immunomodulators directly to infected cells.
Despite these advantages, polypeptides face hurdles in oral bioavailability and proteolytic degradation. Most require parenteral administration, limiting their use outside hospital settings. Strategies to overcome this include PEGylation (attachment of polyethylene glycol) to prolong half-life, or formulation with absorption enhancers for oral delivery. Advances in synthetic biology, such as ribosomal incorporation of non-canonical amino acids, are further expanding the chemical space of therapeutic peptides, enabling designs that resist enzymatic breakdown.
The future of polypeptide drugs lies in hybrid approaches. Combining peptide scaffolds with RNA or small molecules could yield multifunctional conjugates capable of simultaneous pathogen neutralization and immune activation. As computational tools for de novo peptide design improve, the pipeline of clinical candidates will grow, offering new hope against intractable infections. With their blend of specificity, versatility, and reduced resistance risk, polypeptides are poised to play a pivotal role in next-generation antimicrobial therapy.
Delivery Systems: The Make-or-Break Factor for RNA and Peptide Drugs
The therapeutic potential of RNA and peptide drugs is inextricably linked to advances in delivery technologies. Without efficient vectors to shuttle these molecules into target cells, even the most potent sequences or peptides remain ineffective. Lipid nanoparticles (LNPs), the unsung heroes of mRNA vaccines, have set a high bar, but researchers are exploring a menagerie of alternatives to address diverse tissues and diseases. Each platform comes with trade-offs in stability, payload capacity, and immunogenicity, necessitating careful optimization for specific applications.
For RNA therapeutics, LNPs dominate hepatic delivery but struggle elsewhere. To broaden their reach, scientists are tweaking lipid compositions to alter tropism. Ionizable lipids with tailored pKa values can enhance endosomal escape in lung or endothelial cells, while PEGylation patterns influence circulation time. Beyond lipids, polymeric nanoparticles—such as those made from poly(lactic-co-glycolic acid) (PLGA)—offer controlled release profiles, ideal for chronic conditions. In parallel, viral-like particles (VLPs) and exosomes are being harnessed for their natural homing abilities, though manufacturing complexities remain a hurdle.
Peptide drugs face distinct delivery challenges, particularly their susceptibility to proteases and rapid renal clearance. Nanocarriers can shield peptides en route to targets, but covalent modifications often prove more practical. Cyclization, D-amino acid substitutions, and backbone N-methylation are common strategies to thwart enzymatic degradation. For intracellular targets, cell-penetrating peptides (CPPs) like TAT or penetratin facilitate uptake, though off-target effects necessitate careful dosing. Recent work on stimuli-responsive peptides—activated by pH, enzymes, or redox conditions—adds another layer of precision, ensuring activity only at disease sites.
Route of administration also dictates delivery design. Pulmonary delivery of RNA or peptides via dry powder inhalers is gaining traction for respiratory infections, while subcutaneous implants could provide sustained release for chronic diseases. Oral delivery, the holy grail, remains elusive but not impossible. Enteric coatings, protease inhibitors, and permeation enhancers are in development to protect therapeutics through the gastrointestinal tract. Success here could democratize access to these advanced therapies, particularly in resource-limited settings.
The ideal delivery system balances efficacy, safety, and scalability—a trifecta rarely achieved in early iterations. As innovations in biomaterials and bioengineering converge, the next generation of vectors will likely be modular, adaptable to both RNA and peptide payloads. Such platforms could standardize delivery across therapeutic classes, accelerating the translation of lab discoveries to clinic-ready formulations. The race is on to build the perfect vehicle, and the winners will unlock the full potential of nucleic acid and peptide medicine.
Overcoming Immunogenicity: The Silent Challenge in RNA and Peptide Therapies
The very features that make RNA and peptide drugs so potent—their foreignness and biological activity—also risk triggering unwanted immune reactions. Unmodified RNA can activate pattern recognition receptors (PRRs) like TLRs and RIG-I, sparking inflammatory cascades. Similarly, some antimicrobial peptides (AMPs) stimulate cytokine release or elicit neutralizing antibodies, undermining efficacy. Balancing therapeutic activity with immune evasion is a tightrope walk, requiring meticulous molecular design and formulation strategies.
RNA immunogenicity hinges on sequence and modification. Uridine-rich regions are notorious for TLR7/8 activation, while double-stranded RNA byproducts can alert MDA5. To mitigate this, researchers incorporate pseudouridine or N1-methylpseudouridine, which dampen PRR recognition without compromising translation. Codon optimization also plays a role, as rare codons can stall ribosomes, generating aberrant peptides that provoke T-cell responses. For self-amplifying RNA vaccines, which replicate intracellularly, tighter control over replication kinetics is needed to prevent excessive interferon production.
Peptides face analogous hurdles. While human-derived AMPs like defensins are generally tolerated, synthetic or xenobiotic peptides may be immunogenic. Deimmunization strategies include removing T-cell epitopes via in silico prediction tools or grafting therapeutic sequences onto human protein scaffolds. Another approach is to design peptides that mimic “self” motifs, tricking the immune system into ignoring them. For instance, CD4-mimetic peptides in HIV therapy avoid antibody clearance by resembling host MHC-II structures.
Formulation also influences immunogenicity. LNPs, while excellent for RNA delivery, can themselves stimulate complement activation or anti-PEG antibodies. Alternatives like cationic nanoemulsions or sugar-based glassy matrices are under investigation for their stealth properties. For peptides, encapsulation in erythrocyte vesicles or albumin fusion can extend half-life while minimizing immune detection. The goal is to achieve “immune silence” during delivery, reserving immune activation for adjuvanted vaccines where it’s desirable.
The clinical implications of immunogenicity range from reduced efficacy to life-threatening anaphylaxis. Rigorous preclinical screening in humanized mouse models or ex vivo immune assays helps identify risks early. As personalized medicine advances, patient-specific factors—like HLA haplotypes or pre-existing antibodies—may also inform therapeutic design. The future lies in “smart” RNA and peptide constructs that adapt to individual immune profiles, ensuring both safety and potency across diverse populations.
Beyond Infections: RNA and Peptide Drugs in Cancer and Autoimmunity
While infectious diseases have been the proving ground for RNA and peptide therapeutics, their applications in oncology and autoimmunity are equally transformative. Cancer’s genetic heterogeneity and immune evasion tactics make it an ideal target for nucleic acid interventions, while peptides’ precision lends itself to modulating immune checkpoints or tumor microenvironments. The lessons learned from infectious disease research—particularly in delivery and immune modulation—are now being repurposed to tackle these more complex conditions.
In oncology, siRNA and ASOs are silencing oncogenes like KRAS or MYC, long considered “undruggable” by small molecules. mRNA vaccines, meanwhile, are being tailored to express tumor neoantigens, priming the immune system for attack. BioNTech and Moderna, building on their COVID-19 success, have pipelines of individualized cancer vaccines in trials. Another frontier is circular RNA (circRNA), which resists degradation and can express therapeutic proteins persistently, potentially overcoming the transient activity of linear mRNA.
Peptides are making parallel strides. Cyclic peptides like plitidepsin, derived from sea squirts, inhibit eukaryotic elongation factor eEF1A, disrupting protein synthesis in myeloma cells. Others mimic tumor-homing motifs, delivering radionuclides or toxins selectively. Immune checkpoint modulators—peptides that block PD-1/PD-L1 or CTLA-4 interactions—offer an alternative to monoclonal antibodies, with better tissue penetration and lower production costs. The key challenge is achieving sufficient affinity to compete with biologics, which has spurred innovations in stapled and macrocyclic peptides.
Autoimmune diseases represent another frontier. RNA interference (RNAi) can selectively deplete autoreactive B cells by targeting CD20 or BAFF transcripts, offering an alternative to broad immunosuppressants. Peptide-based tolerogenic therapies, such as copolymer-1 for multiple sclerosis, aim to “retrain” the immune system without global suppression. Emerging work on RNA-peptide hybrids, where oligonucleotides are conjugated to autoantigen peptides, could provide dual mechanisms of action—silencing inflammatory genes while restoring immune tolerance.
The versatility of RNA and peptide platforms enables combinatorial approaches unimaginable with traditional drugs. A single LNP could carry siRNAs against oncogenes, mRNAs for tumor antigens, and immune-stimulating peptides, orchestrating a multipronged attack. As these technologies mature, they promise to blur the lines between vaccines, gene therapy, and immunotherapy, creating a new paradigm in precision medicine. The same principles honed against pathogens are now being weaponized against cancer and autoimmunity, proving that biology’s tools are as adaptable as they are powerful.
Manufacturing and Scalability: The Road to Commercial Viability
The transition of RNA and peptide drugs from bench to bedside hinges on solving manufacturing challenges that dwarf those of small molecules. RNA synthesis requires precise nucleotide coupling and capping, while peptides demand iterative amino acid additions and complex purification. Scaling these processes without compromising quality or cost is a formidable task, yet recent innovations are turning what was once artisanal chemistry into streamlined production.
For RNA, the shift from liquid-phase to solid-phase synthesis has been transformative. Automated synthesizers now assemble oligonucleotides stepwise on resin beads, with coupling efficiencies exceeding 99%. Still, the sheer length of mRNA (thousands of nucleotides versus ~20 for ASOs) introduces complexities. Enzymatic synthesis, using T7 RNA polymerase to transcribe DNA templates, is the method of choice for mRNA, but it requires high-purity nucleotide triphosphates and capping analogs. Continuous manufacturing, where reactants flow through reactors rather than batch processing, is emerging as a way to boost yields and consistency.
Peptide synthesis faces its own hurdles, particularly for long or modified sequences. Standard Fmoc (fluorenylmethyloxycarbonyl) chemistry struggles with sequences over 50 residues, often leading to truncated byproducts. Native chemical ligation, where shorter peptides are stitched together, is one workaround. For non-natural amino acids, cell-free translation systems or engineered ribosomes offer an alternative to solid-phase synthesis. Purification, typically via HPLC, remains a bottleneck, driving interest in self-assembling peptides that simplify downstream processing.
The supply chain for raw materials is another critical factor. Nucleoside phosphoramidites for RNA synthesis and protected amino acids for peptides are specialty chemicals with limited suppliers. Diversifying sources and developing more stable intermediates will be key to preventing shortages. Similarly, the lipids used in LNPs were a constraint during the COVID-19 vaccine rollout, spurring efforts to design simpler, more abundant alternatives.
Regulatory harmonization will also shape the future of manufacturing. Current Good Manufacturing Practice (cGMP) guidelines for RNA and peptides are still evolving, particularly for personalized therapies like cancer vaccines. Closed-system bioreactors, single-use disposables, and in-line analytics are becoming standards to ensure reproducibility. As the industry matures, decentralized manufacturing—with regional hubs producing therapies tailored to local outbreaks or cancer profiles—could become feasible, reducing reliance on global supply chains.
The endgame is a manufacturing ecosystem as agile as the therapies themselves. Just as RNA sequences can be swapped to target new pathogens, production lines must adapt rapidly to changing medical needs. Investments now in scalable, modular platforms will pay dividends as RNA and peptide drugs expand from niche applications to mainstream medicine. The promise of these therapies can only be realized if they can be made reliably, affordably, and at scale—a challenge the scientific community is rising to meet.
Ethical and Accessibility Considerations in the New Therapeutic Era
The revolutionary potential of RNA and peptide drugs comes with ethical and logistical dilemmas that mirror their scientific complexities. Who gets access to these often high-cost therapies? How do we balance rapid pandemic response with long-term safety data? And what are the implications of transient gene modulation versus permanent edits? These questions demand thoughtful discourse as these technologies transition from labs to global markets.
Cost is a primary barrier. Current RNA therapeutics, such as patisiran for hereditary transthyretin amyloidosis, carry price tags in the hundreds of thousands annually. Peptide drugs are marginally cheaper but still exceed the reach of many healthcare systems. The expense stems from complex synthesis, proprietary delivery systems, and limited competition. Strategies to reduce costs include open-sourcing non-patentable delivery components, as seen with the LNP formulations shared during COVID-19, or developing generics for older oligonucleotides. Tiered pricing models, where low-income countries pay less, could also improve equity.
Access is another issue. RNA vaccines’ cold-chain requirements initially sidelined regions with poor infrastructure, though thermostable formulations are in development. Peptide drugs, often injectable, face similar hurdles in areas with scarce medical personnel. Self-administered formats, like microneedle patches or oral formulations, could democratize access, but these are years away. Meanwhile, capacity-building initiatives—like mRNA vaccine hubs in Africa—aim to decentralize production, ensuring local autonomy over pandemic responses.
Ethically, the transient nature of RNA drugs offers a middle ground between small molecules and permanent gene therapy. Unlike CRISPR edits, which are irreversible, RNA-mediated effects fade, allowing for dose titration or cessation if adverse events occur. This reversibility is reassuring but raises questions about chronic dosing schedules and patient adherence. For peptides, the line between drug and biologic is blurring, with regulatory agencies grappling with how to classify and approve these hybrid molecules.
Looking ahead, global collaboration will be essential to avoid a therapeutic divide. Patent pools, like the Medicines Patent Pool for HIV drugs, could license RNA and peptide technologies for generic manufacture. Public-private partnerships must also invest in training a workforce skilled in these novel modalities, from bench scientists to regulatory specialists. The goal is a future where cutting-edge therapies are not luxuries for the few, but staples of global health. As RNA and peptide drugs rewrite medicine’s playbook, society must ensure the narrative includes equity as a central theme.
A Molecular Renaissance in Therapeutics
The ascent of RNA and peptide drugs marks a paradigm shift from small-molecule dominance to a new era of programmable, precision medicine. From silencing resistant pathogens to reprogramming immune responses, these modalities offer solutions where traditional drugs falter. Challenges in delivery, manufacturing, and accessibility remain, but the pace of innovation is staggering. As the lines between vaccines, gene therapy, and immunotherapy blur, one thing is clear: the future of medicine will be written in nucleotides and amino acids. The molecules of life are becoming the drugs of tomorrow.
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES

Subscribe
to get our
LATEST NEWS
Related Posts

Medicinal Chemistry & Pharmacology
Polarity Alchemy: Strategic Charge Manipulation in Contemporary Drug Design
The future promises tunable therapies with polarity adjustable by light, magnetic fields, or bioorthogonal triggers.

Medicinal Chemistry & Pharmacology
Metabolic Saboteurs: Precision Drug Design Against Pathological Pathways
The next frontier in precision medicine lies in drugs that surgically disrupt disease-specific metabolic pathways and recalcitrant enzymes.
Read More Articles
Chemical Gale: How Wind Energy is Reshaping Industrial Manufacturing
The integration of wind energy into chemical manufacturing constitutes a fundamental reimagining of process chemistry.