Immunotherapy Redefined: Cancer Vaccines as a Cornerstone of Prostate Cancer Treatment
Prostate cancer remains the most prevalent malignancy in aging men, often progressing to advanced, treatment-resistant stages despite the efficacy of traditional therapies like androgen deprivation therapy (ADT). This grim trajectory underscores the need for novel treatment paradigms. Immunotherapy, which leverages the body’s immune system to target and eliminate cancer cells, has emerged as a beacon of hope. Among its strategies, cancer vaccines stand out due to their specificity, safety, and potential to generate long-lasting immune memory.
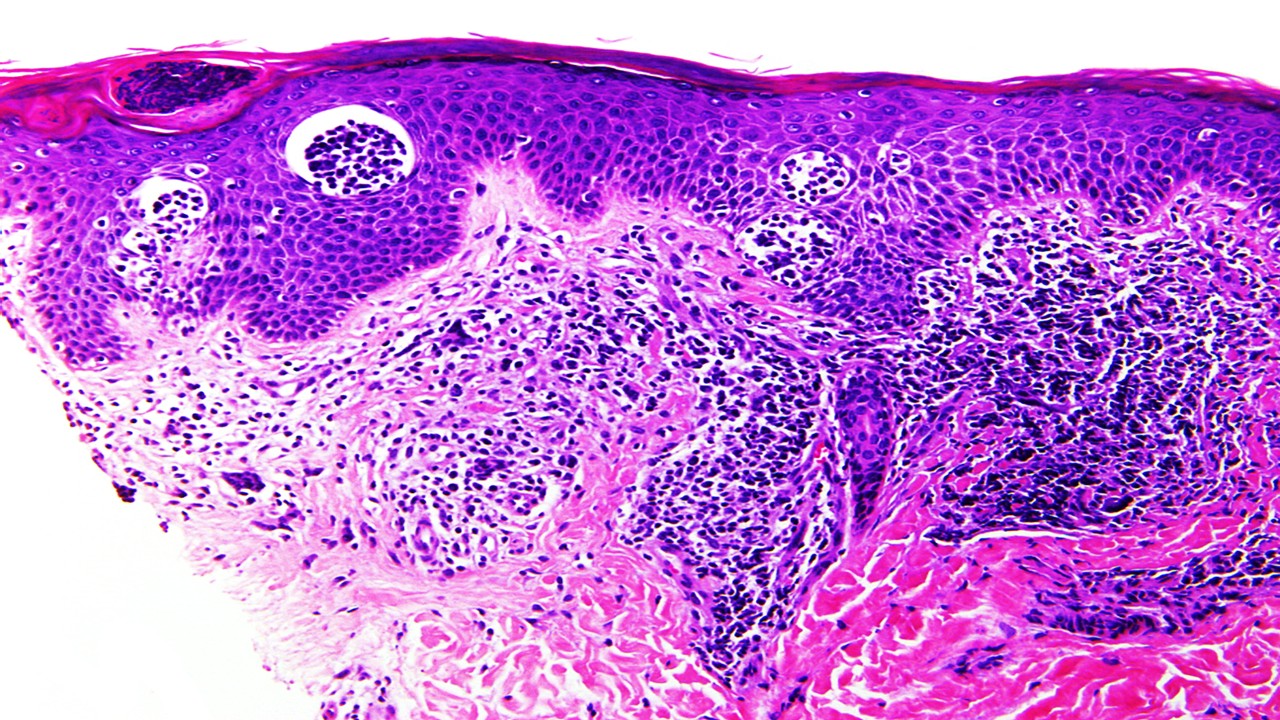
Unlike other immunotherapeutic approaches, cancer vaccines introduce tumor antigens into the body, stimulating T-cell responses that specifically target and destroy cancer cells. This precision makes them particularly appealing for cancers like prostate cancer, which often exhibit low immunogenicity. The U.S. Food and Drug Administration’s approval of Sipuleucel-T as the first cancer vaccine for metastatic castration-resistant prostate cancer (mCRPC) marked a turning point, highlighting the clinical potential of vaccines in this challenging disease. However, the complex immunosuppressive microenvironment of prostate tumors, coupled with patient-specific factors like age and hormonal levels, has tempered the success of single-agent vaccine therapies.
Cancer vaccines are not a monolithic entity. They encompass diverse platforms, including dendritic cell vaccines, viral-based therapies, peptide vaccines, and innovative DNA and mRNA-based approaches. These vaccines differ in their mechanisms but share a common goal: to convert the immune system into a precise weapon against prostate cancer. As research progresses, combination therapies that pair vaccines with other modalities like immune checkpoint inhibitors, radiotherapy, or traditional therapies are gaining momentum, offering a multi-pronged approach to tackle the disease’s inherent resistance mechanisms.
Sipuleucel-T: Pioneering the Path for Dendritic Cell Vaccines
Sipuleucel-T, a dendritic cell-based vaccine, has set the benchmark for prostate cancer immunotherapy. By leveraging the patient’s immune cells, this vaccine introduces a fusion protein comprising prostate acid phosphatase (PAP) and granulocyte-macrophage colony-stimulating factor (GM-CSF), effectively activating T cells to elicit an anti-tumor response. Clinical trials have demonstrated its ability to prolong overall survival in patients with mCRPC, despite minimal impact on progression-free survival.
The vaccine’s efficacy appears most pronounced when administered early in the disease course. Patients with lower baseline prostate-specific antigen (PSA) levels benefit significantly, likely due to a less immunosuppressive tumor environment and enhanced antigen-presenting cell (APC) activation. This highlights the importance of patient stratification in maximizing therapeutic outcomes. Real-world data further corroborates these findings, showing extended survival when Sipuleucel-T is combined with second-generation anti-androgen therapies.
However, the success of Sipuleucel-T is tempered by practical challenges, including high treatment costs and limited clinical efficacy as a standalone therapy. This has spurred investigations into combination strategies. Trials pairing Sipuleucel-T with androgen deprivation therapy, radiotherapy, or immune checkpoint inhibitors have shown promise, with some enhancing T-cell responses and reducing tumor burden. These findings underscore the potential of integrating Sipuleucel-T into multi-modal regimens to amplify its therapeutic impact.
Peptide and Nucleic Acid Vaccines: Precision Tools for Immune Activation
Peptide vaccines represent a straightforward yet powerful approach to prostate cancer immunotherapy. By targeting specific tumor antigens or cell surface proteins, these vaccines aim to enhance the immune system’s capacity to identify and eliminate cancer cells. Clinical trials have demonstrated their ability to reduce PSA levels and induce both cellular and humoral immune responses. However, their efficacy in extending survival remains inconsistent, often influenced by patient-specific factors like baseline immune profiles.
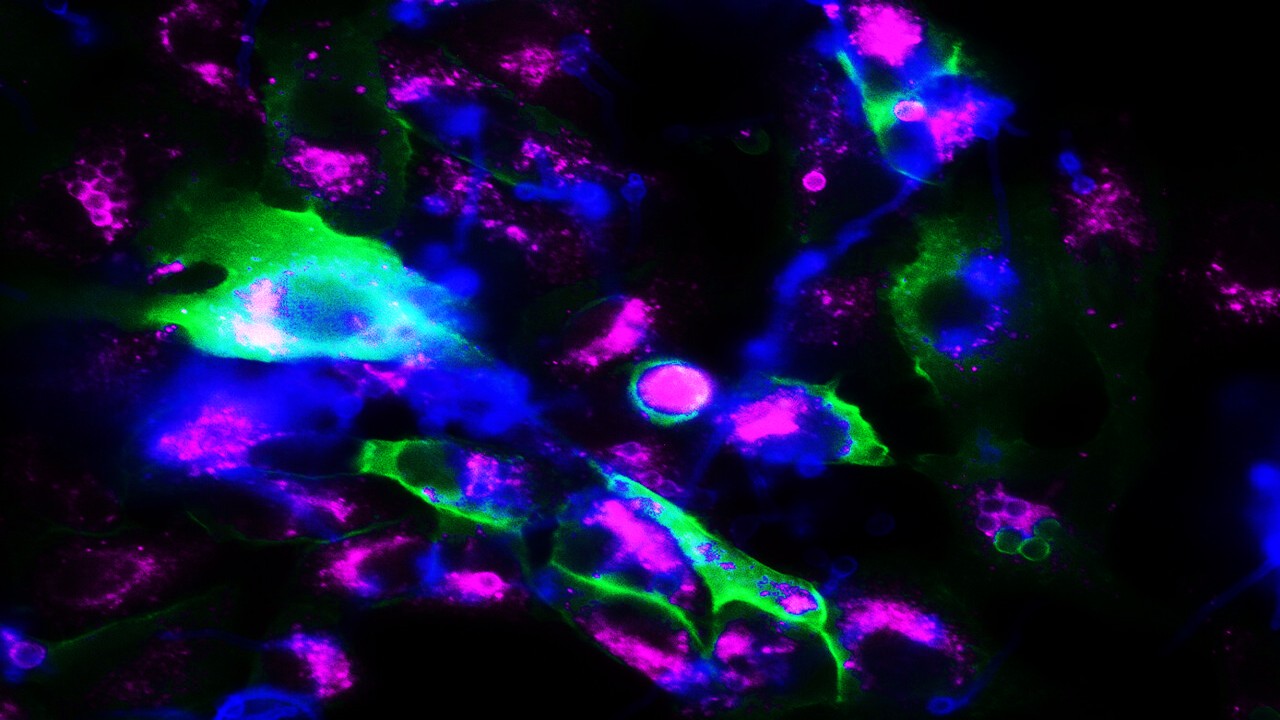
Advances in bioinformatics have revitalized interest in peptide vaccines, enabling the design of personalized neoantigen-based therapies. These individualized vaccines leverage tumor-specific mutations to generate highly targeted immune responses, potentially overcoming the limitations of traditional peptide approaches. Despite these advancements, challenges like limited adjuvant options and the immunosuppressive tumor microenvironment continue to hinder their widespread application.
Nucleic acid vaccines, particularly DNA and RNA-based platforms, offer a versatile alternative. These vaccines deliver genetic blueprints for tumor antigens, enabling the host’s cells to produce and present these proteins to the immune system. DNA vaccines, such as those targeting PAP or PSA, have shown promise in early trials, eliciting robust T-cell responses and slowing disease progression. RNA vaccines, like CV9103 and CV9104, represent a newer frontier, boasting advantages like non-infectious expression and simultaneous multi-antigen targeting. Although clinical outcomes for these vaccines have been mixed, ongoing research integrating checkpoint inhibitors and advanced antigen screening techniques holds promise for enhancing their efficacy.
Viral and Cellular Vaccines: Engineering the Future of Immunotherapy
Viral-based vaccines, such as PROSTVAC, utilize modified viruses to deliver tumor antigens and stimulate a robust immune response. These vaccines have demonstrated significant survival benefits in phase II trials, but phase III results have been less conclusive, highlighting the need for optimized delivery and combination strategies. Innovations in adenoviral vectors and listeria-based vaccines are expanding the possibilities for viral platforms, offering enhanced immunogenicity and safety profiles.
Cellular vaccines, including GVAX, take a different approach by using genetically modified cancer cells to elicit an immune response. Early-phase trials have shown promising PSA reductions and immune activation. However, large-scale studies have faced setbacks, with limited survival benefits and safety concerns. These challenges underscore the complexity of developing effective cellular vaccines, necessitating further refinement and integration with other therapeutic modalities.
Combination Therapies: Amplifying the Immune Response
Prostate cancer’s inherent resistance to immunotherapy often necessitates combination approaches. Pairing vaccines with immune checkpoint inhibitors like anti-PD-1 or CTLA-4 antibodies has shown potential to overcome immune evasion mechanisms, enhancing T-cell infiltration and activity. Similarly, radiotherapy can synergize with vaccines by converting “cold” tumors into “hot” tumors, making them more susceptible to immune attack.
Chemotherapy and hormonal therapies also offer complementary benefits. By reducing tumor burden and modulating the immune microenvironment, these treatments can enhance vaccine efficacy. Ongoing trials are exploring various combinations, seeking to identify optimal regimens that balance efficacy and safety. The success of these strategies will likely depend on precision medicine approaches, leveraging biomarkers to guide patient selection and treatment sequencing.
The Road Ahead: Challenges and Opportunities
Despite significant progress, the clinical adoption of prostate cancer vaccines faces several hurdles. The tumor’s immunosuppressive microenvironment, inter-patient variability, and the high cost of vaccine development remain substantial barriers. Moreover, the lack of standardized protocols for vaccine administration and the need for large-scale validation studies further complicate their integration into routine clinical practice.
Advancements in sequencing technologies and bioinformatics are paving the way for more personalized approaches, enabling the rapid identification and synthesis of patient-specific tumor neoantigens. These innovations, coupled with the integration of multi-omics data, hold the potential to revolutionize prostate cancer immunotherapy, transforming it into a truly individualized science.
The future of prostate cancer vaccines lies in combination therapies that harness the strengths of multiple modalities. By addressing the disease’s inherent resistance mechanisms and tailoring treatments to individual patient profiles, these approaches promise to deliver more durable and meaningful clinical outcomes. As research continues to unravel the complexities of prostate cancer immunotherapy, the vision of vaccines as a cornerstone of treatment becomes increasingly attainable.
Study DOI: https://doi.org/10.3390/vaccines12121384
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES

Subscribe
to get our
LATEST NEWS
Related Posts

Infectious Diseases & Vaccinology
Enduring Blockade: Five-Year Functional Antibody Persistence Against Emerging GII.4 and GII.17 Noroviruses
Natural infection with dominant GII noroviruses elicits long-lived functional antibodies, redefining immune durability in viral gastroenteritis.
Infectious Diseases & Vaccinology
Resistant Mycosis: Reimagining Antifungal Therapy Through Mechanistic Innovation and Molecular Disruption
Emerging antifungal strategies are redefining treatment by targeting fungal physiology through diversified, mechanism-driven approaches that overcome entrenched drug resistance.
Infectious Diseases & Vaccinology
Fungal Refractory States: Deciphering Pathobiology and Therapeutic Weaknesses in the Era of Rising Antifungal Resistance
Rising antifungal resistance reflects a multidimensional biological challenge that demands mechanistically innovative, host-integrated therapeutic strategies.

Infectious Diseases & Vaccinology
Epigenetic Parasite Vulnerabilities: Repurposing Histone Deacetylase Inhibitors for Complex Multispecies Therapeutics
Repurposed HDAC inhibitors target essential parasite epigenetic machinery, offering a powerful but complex frontier for next-generation antiparasitic therapy.
Read More Articles
Spatial Collapse: Pharmacologic Degradation of PDEδ to Disrupt Oncogenic KRAS Membrane Localization
PDEδ degradation disrupts KRAS membrane localization to collapse oncogenic signaling through spatial pharmacology rather than direct enzymatic inhibition.
Neumedics’ Integrated Innovation Model: Dr. Mark Nelson on Translating Drug Discovery into API Synthesis
Dr. Mark Nelson of Neumedics outlines how integrating medicinal chemistry with scalable API synthesis from the earliest design stages defines the next evolution of pharmaceutical development.
Zentalis Pharmaceuticals’ Clinical Strategy Architecture: Dr. Stalder on Data Foresight and Oncology Execution
Dr. Joseph Stalder of Zentalis Pharmaceuticals examines how predictive data integration and disciplined program governance are redefining the future of late-stage oncology development.
Exelixis Clinical Bioanalysis Leadership, Translational DMPK Craft, and the Kirkovsky Playbook
Senior Director Dr. Leo Kirkovsky brings a rare cross-modality perspective—spanning physical organic chemistry, clinical assay leadership, and ADC bioanalysis—to show how ADME mastery becomes the decision engine that turns complex drug systems into scalable oncology development programs.
Policy Ignition: How Institutional Experiments Become Durable Global Evidence for Pharmaceutical Access
Global pharmaceutical access improves when IP, payment, and real-world evidence systems are engineered as interoperable feedback loops rather than isolated reforms.







