Malaria: A Global Challenge Unmet by Current Vaccine Modalities
Malaria remains a tenacious global health burden, claiming hundreds of thousands of lives annually despite existing preventive measures. The cornerstone of malaria immunization, subunit vaccines such as RTS,S/AS01 (Mosquirix) and R21, target the Plasmodium falciparum circumsporozoite protein (CSP), a major antigen expressed during the sporozoite stage. These vaccines offer transient efficacy, with protective rates declining significantly after one year. Among infants in highly endemic regions, the efficacy is even lower compared to older children, further highlighting the urgent need for alternative strategies.
The limitations of subunit vaccines stem from their narrow antigenic focus and relatively weak induction of durable immunity. CSP-targeted immunity provides partial protection but fails to fully mimic the complex immune responses elicited by natural infection, where multiple antigens are presented sequentially throughout the parasite’s lifecycle. This antigenic limitation underscores the need for vaccination approaches that expose the immune system to a broader array of P. falciparum antigens.
Whole-sporozoite-based strategies represent a paradigm shift in malaria vaccine development. Unlike subunit vaccines, genetically or radiation-attenuated sporozoites (GAS or RAS) simulate the early stages of natural infection, activating a multifaceted immune response. However, radiation-attenuated sporozoites often require impractically high doses to achieve meaningful protection. A novel approach, involving late-liver-stage genetically attenuated parasites, seeks to overcome these challenges by extending antigenic exposure and eliciting stronger, more durable immune responses.
The Complex Pathophysiology of Malaria: An Interplay of Host and Parasite
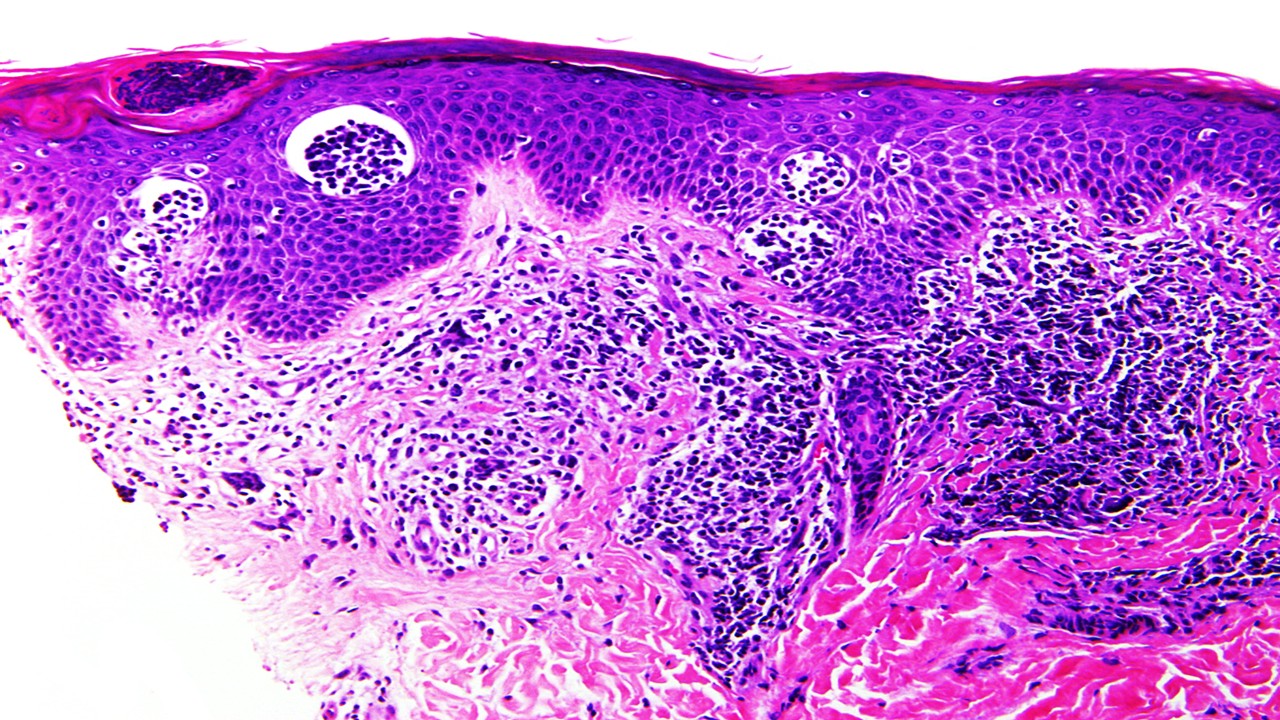
Malaria pathophysiology is driven by the Plasmodium parasite’s complex lifecycle and its intricate interactions with the human host. The disease begins when an infected female Anopheles mosquito inoculates sporozoites into the dermis during a blood meal. These sporozoites rapidly migrate to the liver via the bloodstream, where they invade hepatocytes and undergo asexual replication to form thousands of merozoites. This pre-erythrocytic stage is clinically silent but critical for establishing infection. The liver stage lasts approximately 7–10 days, after which merozoites are released into the bloodstream, marking the onset of symptomatic disease.
Once in circulation, merozoites invade erythrocytes and initiate the intraerythrocytic developmental cycle, where asexual reproduction continues. The parasite’s progression through the ring, trophozoite, and schizont stages within red blood cells is synchronized, leading to periodic bursts of merozoites and the release of inflammatory mediators. These cyclic events correlate with the characteristic fever paroxysms seen in malaria. During this stage, infected erythrocytes display parasite-derived proteins on their surface, such as Plasmodium falciparum erythrocyte membrane protein 1 (PfEMP1), which mediates cytoadherence to vascular endothelial cells. This sequestration prevents infected erythrocytes from being cleared by the spleen but contributes to complications such as cerebral malaria and placental malaria by obstructing microcirculation.
The host immune response to malaria is a double-edged sword. While it plays a vital role in controlling parasitemia, it also contributes to pathogenesis. The activation of macrophages, dendritic cells, and T cells leads to the release of proinflammatory cytokines such as tumor necrosis factor-alpha (TNF-α), interleukin-1 beta (IL-1β), and interferon-gamma (IFN-γ). These cytokines drive fever, malaise, and other systemic symptoms. In severe malaria, excessive immune activation can result in endothelial dysfunction, capillary leak syndrome, and multi-organ failure. The parasite’s ability to evade immune detection through antigenic variation and other immune-evasion strategies further complicates disease resolution, leading to persistent infections and immune exhaustion in chronic cases. Understanding these pathophysiological mechanisms is crucial for developing targeted therapies and effective vaccines, such as GA2, which aim to disrupt key stages of the parasite’s lifecycle.
The Trial Design: Engineering Late-Liver-Stage Arrest in P. falciparum
The trial evaluated a second-generation genetically attenuated parasite (GAP), designated GA2, which is a P. falciparum sporozoite modified to arrest late during its intrahepatic development. This parasite carries a mei2 single-gene knockout, halting its progression six days after hepatocyte invasion. Unlike earlier GAPs, such as GA1, which arrest within 24 hours, GA2 provides extended antigenic exposure in the liver, hypothesized to enhance protective efficacy.
The study was conducted in two stages at Leiden University Medical Center and Radboud University Medical Center. Stage A employed an open-label, dose-escalation design to assess the safety of immunization with GA2. Participants were exposed to 15 or 50 mosquito bites from Anopheles stephensi mosquitoes infected with GA2. Stage B, a double-blind, randomized trial, compared the efficacy of GA2 to GA1 and a placebo (uninfected mosquito bites) after three immunization sessions, each involving 50 bites administered at 28-day intervals.
Controlled human malaria infection (CHMI) followed three weeks post-immunization. All participants in Stage B received five bites from mosquitoes infected with unattenuated P. falciparum (Pf3D7 strain). Primary endpoints included the incidence and severity of adverse events and the detection of blood-stage parasitemia using qPCR. Secondary endpoints assessed humoral and cellular immune responses, with a focus on polyfunctional T-cell induction. The trial protocol adhered to strict ethical and regulatory standards, ensuring participant safety and data integrity.
Immune Mechanisms: Polyfunctional T Cells and Antibody Profiles
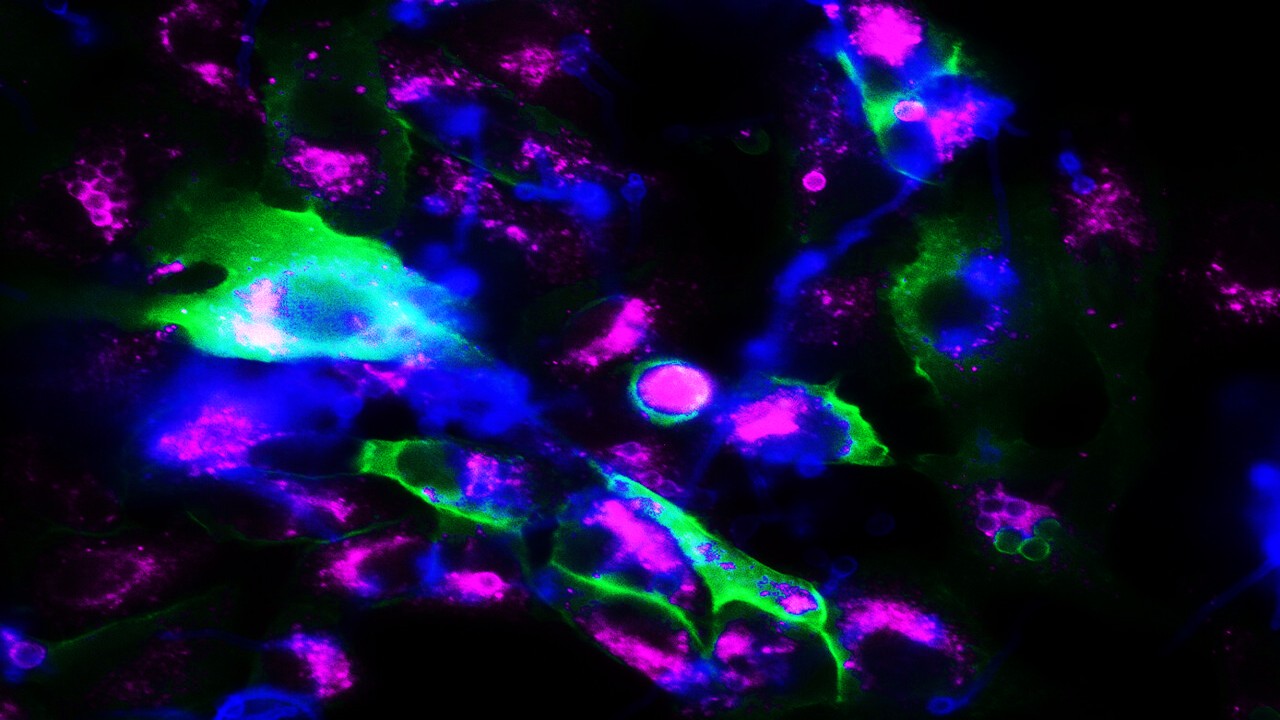
The results revealed that GA2-induced immunization provided 89% protection against controlled malaria infection, significantly outperforming GA1 (13%) and placebo (0%). The extended liver-stage arrest of GA2 enabled robust activation of both humoral and cellular immune pathways. While antibody titers targeting CSP were elevated in both GA1 and GA2 recipients, protective immunity was not correlated with CSP-specific antibodies. Instead, cellular immunity emerged as the defining factor.
Participants immunized with GA2 displayed a marked increase in polyfunctional CD4+ T cells expressing cytokines such as interferon-γ, TNF-α, and interleukin-2. These effector memory T cells exhibited a proinflammatory signature essential for parasite clearance. Additionally, GA2 uniquely induced Vδ2+ γδ T cells, a subset associated with protective immunity. These cells demonstrated polyfunctional cytokine expression, further differentiating GA2 from its early-arresting counterpart.
Interestingly, late-liver-stage arrest in GA2 did not translate to detectable antibodies against downstream antigens like apical membrane antigen 1 (AMA1) or merozoite surface protein 1 (MSP1). This finding underscores the potential for liver-stage antigens to prime robust cellular responses independently of humoral immunity. The lack of detectable P. falciparum–specific CD8+ T cells in peripheral blood, while consistent with prior studies, leaves open questions about the role of liver-resident memory T cells in protective efficacy.
Safety Profile and Implications for Broader Deployment
The trial reported no serious adverse events across all groups. Localized erythema and pruritus at bite sites were the most common adverse effects, resolving without complications. Systemic reactions, such as mild headache or myalgia, occurred at low frequencies and were self-limiting. Importantly, no breakthrough blood-stage infections were observed in participants exposed to up to 50 bites from GA2-infected mosquitoes, confirming the attenuation stability of the mei2 knockout.
Two participants exhibited transient troponin T elevations, deemed unrelated to the intervention, while another showed elevated liver function tests likely caused by antihistamine use. These isolated events underscore the importance of rigorous safety monitoring in vaccine trials. The absence of breakthrough infections aligns with preclinical findings, reinforcing GA2’s safety as a candidate for broader evaluation.
Scaling GA2 immunization for malaria-endemic regions will require overcoming logistical barriers. The reliance on mosquito bites for sporozoite delivery limits feasibility, necessitating advancements in scalable manufacturing methods, such as injectable formulations. Additionally, long-term studies are needed to assess the durability of GA2-induced protection and its efficacy against diverse P. falciparum strains in endemic settings.
Toward Next-Generation Malaria Vaccines
The high protective efficacy observed with GA2 represents a significant advancement in malaria vaccine development. By leveraging extended antigenic exposure during the liver stage, GA2 elicits potent cellular immune responses that surpass those induced by earlier vaccine candidates. This innovative approach aligns with the broader goal of developing a vaccine capable of sustained efficacy across diverse populations and transmission settings.
Future research must address key gaps, including the role of liver-resident memory T cells and the mechanisms underlying γδ T-cell induction. Expanding the scope of trials to include malaria-endemic regions will provide critical insights into GA2’s real-world applicability. Furthermore, integrating GA2 with other immunization strategies, such as heterologous prime-boost regimens, could enhance both breadth and durability of protection.
In the fight against malaria, late-liver-stage attenuated sporozoites like GA2 offer a transformative pathway toward achieving lasting immunity. This milestone underscores the potential of next-generation vaccines to address one of humanity’s most enduring public health challenges.
Study DOI: 10.1056/NEJMoa2313892
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES

Subscribe
to get our
LATEST NEWS
Related Posts

Infectious Diseases & Vaccinology
Enduring Blockade: Five-Year Functional Antibody Persistence Against Emerging GII.4 and GII.17 Noroviruses
Natural infection with dominant GII noroviruses elicits long-lived functional antibodies, redefining immune durability in viral gastroenteritis.
Infectious Diseases & Vaccinology
Resistant Mycosis: Reimagining Antifungal Therapy Through Mechanistic Innovation and Molecular Disruption
Emerging antifungal strategies are redefining treatment by targeting fungal physiology through diversified, mechanism-driven approaches that overcome entrenched drug resistance.
Infectious Diseases & Vaccinology
Fungal Refractory States: Deciphering Pathobiology and Therapeutic Weaknesses in the Era of Rising Antifungal Resistance
Rising antifungal resistance reflects a multidimensional biological challenge that demands mechanistically innovative, host-integrated therapeutic strategies.

Infectious Diseases & Vaccinology
Epigenetic Parasite Vulnerabilities: Repurposing Histone Deacetylase Inhibitors for Complex Multispecies Therapeutics
Repurposed HDAC inhibitors target essential parasite epigenetic machinery, offering a powerful but complex frontier for next-generation antiparasitic therapy.
Read More Articles
Spatial Collapse: Pharmacologic Degradation of PDEδ to Disrupt Oncogenic KRAS Membrane Localization
PDEδ degradation disrupts KRAS membrane localization to collapse oncogenic signaling through spatial pharmacology rather than direct enzymatic inhibition.
Neumedics’ Integrated Innovation Model: Dr. Mark Nelson on Translating Drug Discovery into API Synthesis
Dr. Mark Nelson of Neumedics outlines how integrating medicinal chemistry with scalable API synthesis from the earliest design stages defines the next evolution of pharmaceutical development.
Zentalis Pharmaceuticals’ Clinical Strategy Architecture: Dr. Stalder on Data Foresight and Oncology Execution
Dr. Joseph Stalder of Zentalis Pharmaceuticals examines how predictive data integration and disciplined program governance are redefining the future of late-stage oncology development.
Exelixis Clinical Bioanalysis Leadership, Translational DMPK Craft, and the Kirkovsky Playbook
Senior Director Dr. Leo Kirkovsky brings a rare cross-modality perspective—spanning physical organic chemistry, clinical assay leadership, and ADC bioanalysis—to show how ADME mastery becomes the decision engine that turns complex drug systems into scalable oncology development programs.
Policy Ignition: How Institutional Experiments Become Durable Global Evidence for Pharmaceutical Access
Global pharmaceutical access improves when IP, payment, and real-world evidence systems are engineered as interoperable feedback loops rather than isolated reforms.







