Decoding CKD: Beyond Traditional Markers
Chronic kidney disease (CKD) has long been defined by its progressive nature, with clinical management focusing on its most visible endpoints: reduced glomerular filtration rate (eGFR) and overt albuminuria. However, these traditional diagnostic markers often emerge only after significant renal damage has occurred, making early intervention a formidable challenge. As CKD silently progresses through its stages, the disease’s molecular underpinnings remain poorly understood, particularly in its nascent phases.
This knowledge gap has historically hindered the identification of effective therapeutic interventions that target the root causes of CKD progression. Most available treatments focus on managing symptoms or slowing decline, rather than addressing the molecular drivers of kidney dysfunction. Recent research on plasma proteomics, however, provides a crucial breakthrough. By mapping protein abundance across CKD stages, this study reveals how distinct molecular events unfold in the early stages of CKD.
Stage 2, in particular, emerges as a critical turning point. This is where subtle biochemical disruptions first coalesce into systemic pathophysiological changes. The findings suggest that CKD does not progress in a linear fashion but rather pivots sharply at this stage, driven by an interplay of inflammatory, angiogenic, and tissue-regenerative processes. Understanding these mechanisms in finer detail is key to rethinking both diagnosis and treatment.
Stage 2 CKD: Where Molecular Chaos Begins
While Stage 1 CKD is often characterized by mild structural changes and a slight reduction in renal function, Stage 2 represents a tipping point where these changes accelerate and become molecularly evident. Proteomic analysis identifies dramatic shifts in protein expression, with marked activation of pathways that govern immune response, tissue repair, and vascular remodeling. These disruptions highlight Stage 2 as the moment when CKD transitions from silent dysfunction to active pathology.
One of the most striking findings in Stage 2 is the activation of inflammatory pathways. Elevated levels of complement proteins, including C3 and C factor B, signal an overactive immune response. These proteins are known to mediate complement cascade activation, which exacerbates renal tissue damage through autoimmune-like mechanisms. Reduced levels of protective inhibitors, such as C factor H, further accelerate this inflammatory process, setting the stage for chronic immune activation.
Simultaneously, vascular health begins to deteriorate in Stage 2. Proteins such as vascular cell adhesion protein 1 (VCAM-1) are uniquely elevated at this stage, facilitating leukocyte migration into renal tissues and worsening inflammation. This molecular profile suggests that Stage 2 CKD is not merely a progression of renal dysfunction but an orchestrated escalation of pathological processes. These findings underscore the importance of intervening early to arrest disease progression at its molecular root.
Inflammation: The Smoldering Fire
Inflammation emerges as a central driver of CKD progression, with its impact becoming particularly pronounced in Stage 2. While inflammation is a protective response to acute injury, its chronic activation in CKD fuels a vicious cycle of tissue damage and immune dysregulation. Plasma proteomic data show a peak in the abundance of acute-phase reactants, such as haptoglobin and serum amyloid A, during Stage 2, amplifying systemic inflammatory signals.
Complement activation plays a pivotal role in this inflammatory cascade. The study identifies disruptions in multiple complement pathways, including the alternative and lectin pathways, which converge to exacerbate renal injury. For instance, the decline in MASP-2 abundance, a regulator of the lectin pathway, weakens the kidney’s ability to resolve inflammation, while elevated C3 levels promote further tissue damage. This imbalance creates an environment in which renal function deteriorates rapidly, as inflammation becomes self-perpetuating.
Adding complexity to this scenario is the role of adhesion molecules like VCAM-1, which act as molecular gateways for leukocytes to infiltrate renal tissues. This infiltration worsens localized inflammation and accelerates fibrosis, a hallmark of advanced CKD. By targeting these inflammatory mediators, particularly in Stage 2, clinicians may be able to prevent the cascade of events that lead to irreversible renal damage.
Angiogenesis: A Pathway in Flux
The role of angiogenesis in CKD is paradoxical, oscillating between repair and pathology. During Stage 2, angiogenic pathways become overactive, as evidenced by elevated levels of angiogenin (ANG) and neuropilin-1 (NRP-1). These proteins, while essential for vascular remodeling, can also contribute to glomerular dysfunction when dysregulated.
ANG, for instance, promotes the formation of new blood vessels, a process critical for tissue repair. However, its overabundance in Stage 2 disrupts the balance between vessel growth and stability, leading to leaky capillaries that impair renal filtration. Similarly, NRP-1, a co-receptor involved in endothelial cell signaling, sees a sharp rise during this stage. While NRP-1 is protective in moderation, its excessive activity can damage the glomerular basement membrane, compounding kidney injury.
Another notable player is β3 integrin, a molecule critical for angiogenesis signaling. Proteomic data show its abundance peaking in Stage 2, correlating with increased vascular activity. While these angiogenic responses are initially adaptive, their persistence in CKD creates a pathological environment that accelerates disease progression. These findings highlight angiogenesis as a potential therapeutic target, with interventions aimed at restoring balance in vascular remodeling pathways.
Tissue Repair: When Healing Turns Harmful
The kidney’s ability to repair itself is both a blessing and a curse. In Stage 2 CKD, tissue repair mechanisms are activated in response to injury, but their dysregulation leads to maladaptive outcomes. Proteins such as cofilin-1 and vitamin D binding protein (DBP) show elevated levels, indicating active cytoskeletal remodeling and immune modulation. However, this heightened activity also triggers the early stages of fibrosis.
Fibrosis, characterized by excessive deposition of extracellular matrix proteins, begins to take hold during Stage 2. Lumican, a pro-inflammatory matrix protein, is significantly elevated, signaling a shift from repair to scarring. This molecular change is accompanied by increases in other fibrosis-associated proteins, such as pigment epithelium-derived factor (PEDF), which, despite its protective properties, can contribute to chronic tissue remodeling.
Interestingly, the study also identifies alpha-2-macroglobulin (A2M) as a key player in tissue repair during Stage 2. A2M, known for its anti-inflammatory properties, is elevated during this stage, suggesting an attempt by the kidney to counteract the ongoing damage. However, this compensatory response is ultimately overwhelmed by the persistent inflammatory and fibrotic signals, underscoring the need for early intervention.
Lipid Dysregulation: A Cardiovascular Connection
Lipid metabolism undergoes significant disruptions in CKD, with these changes becoming apparent as early as Stage 2. Elevated levels of apolipoproteins, particularly apoA-IV, reflect a maladaptive response to kidney dysfunction. While these proteins play essential roles in lipid transport, their accumulation contributes to the formation of atherogenic particles, increasing cardiovascular risk.
The proteomic data reveal peaks in lipoprotein metabolism pathways during Stages 1 and 2, suggesting that these disruptions are among the earliest systemic effects of CKD. ApoA-I and apoA-II, for instance, show elevated levels, indicating a shift in lipid processing. However, as CKD progresses, these compensatory mechanisms fail, leading to lipid accumulation and further renal damage.
These findings emphasize the interconnected nature of CKD and cardiovascular disease. By addressing lipid dysregulation in the early stages of CKD, clinicians may be able to reduce not only renal progression but also the risk of cardiovascular complications, a major cause of mortality in CKD patients.
Redefining CKD Progression
This study redefines our understanding of CKD by positioning Stage 2 as the critical juncture where molecular disruptions accelerate disease progression. By identifying the specific pathways activated during this stage, researchers have laid the groundwork for targeted interventions that could halt CKD in its tracks.
From inflammation and angiogenesis to tissue repair and lipid metabolism, the molecular events of Stage 2 provide a roadmap for both diagnosis and treatment. The challenge now lies in translating these findings into clinical practice, with the hope of improving outcomes for the millions of individuals affected by CKD worldwide.
Study DOI: https://doi.org/10.3390/biomedicines10071522
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES

Subscribe
to get our
LATEST NEWS
Related Posts
Chronic & Debilitating Diseases
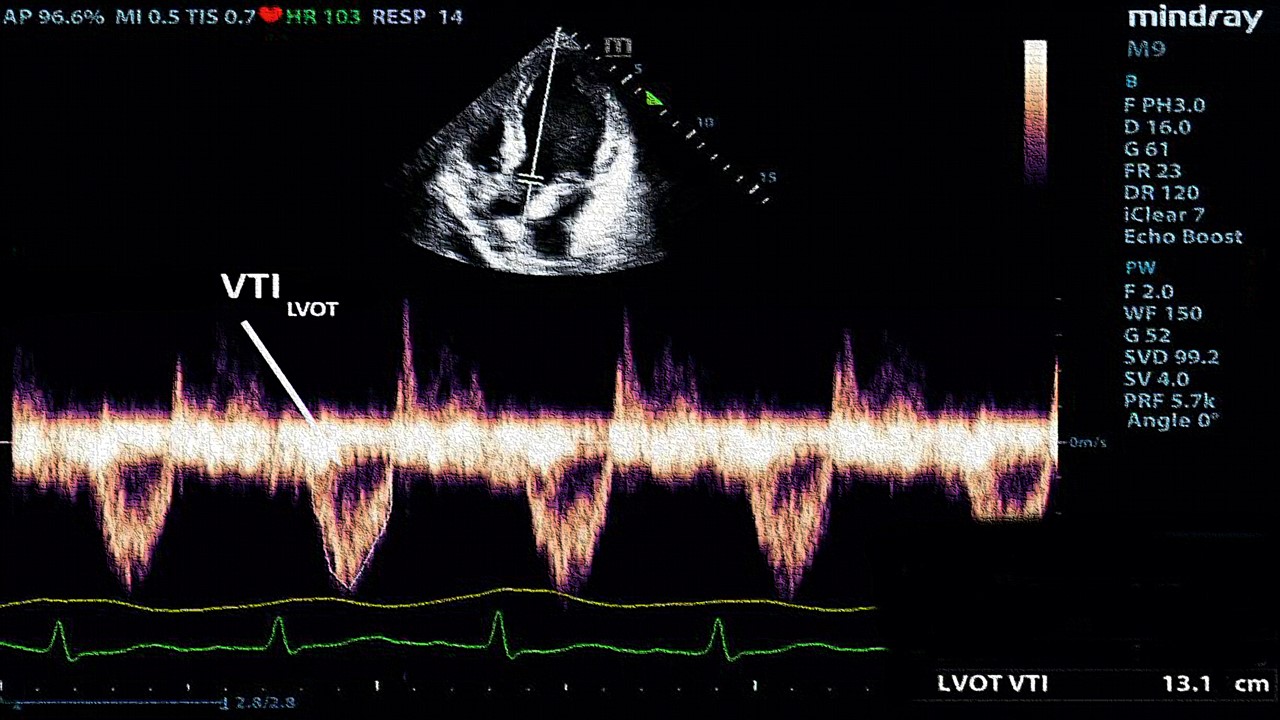
A New Lens on Shock: Hemodynamic Insights Through Critical Care Ultrasound
CCU has transformed the hemodynamic assessment of shock, delivering a reliable, reproducible, and non-invasive tool for ICU clinicians.

Chronic & Debilitating Diseases
Silent Signals: The Enigma of MINOCA and INOCA in Modern Cardiology
The intricate relationship between MINOCA and INOCA highlights the multifaceted nature of ischemic heart disease (IHD).
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.