Parkinsonism is a prevalent movement disorder that is characterized by abnormalities in associated brain regions as well as dysfunction of the basal ganglia. Skeletal muscle rigidity, akinesia (or bradykinesia), a flat face, and resting tremor are the four hallmarks of Parkinson’s disease. In progressive parkinsonism, personality changes, psychosis, and hallucinations are possible.
The disease is incurable, is generally progressive, and leads to increasing disability with time, but pharmacologic treatment may relieve motor symptoms and improve the quality of life for many years.
Naturally Occurring Parkinsonism
The aging process causes the naturally occurring disease, whose origin is unknown, to manifest itself more frequently starting in the fifth or sixth decade of a person’s existence. A sizable portion of patients have detectable mutations in the parkin or synuclein genes. Autosomal dominant parkinsonism may also result from mutations in the UCHL1 gene and the leucine-rich repeat kinase 2 (LRRK2) gene at 12cen.
Another evidence supporting the idea that Parkinson’s disease may be a prion illness came from the discovery of Lewy bodies, which are intracellular inclusion bodies containing α-synuclein, in embryonic dopaminergic cells grafted into the brains of parkinsonian patients some years previously.
NSAID users who use them regularly experience a drop in Parkinsonian incidence, but farmers and those exposed to lead or manganese experience an elevation. A decline in striatal dopamine levels and the loss of dopaminergic neurons in the nigrostriatal tract, which typically block the functioning of striatal GABAergic neurons, are pathologic features. In GABAergic neuronal cells, the majority of the postsynaptic dopaminergic neurons are of the D2 subtype (negatively associated to adenylyl cyclase), while D3 receptors might possibly be important. Dopamine and acetylcholine processes are out of balance in parkinsonism because normal dopaminergic neurotransmission is reduced, which causes excessive excitatory responses of cholinergic neurons on striatal GABAergic neurons.
Drug-Induced Parkinsonism
The movement disorders symptoms that many medicines might produce are typically reversible. The antipsychotic medications butyrophenone and phenothiazine, which inhibit brain dopamine receptors, represent the most significant precipitating substances. Similar symptoms are brought on by reserpine at larger concentrations, most likely due to dopamine depletion in the brain. By destroying dopaminergic neurons in the nigrostriatal tract, 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP), a chemical byproduct of an illegal meperidine analog’s unsuccessful manufacture, results in permanent parkinsonism. Animals administered with type B MAOI are shielded from the neurotoxicity of MPTP.
Drug Therapy of Parkinsonism
Boosting dopamine levels in the brain, reducing muscarinic cholinergic neuronal activity, or both are possible pharmacological therapy options for parkinsonism. Whereas the substantia nigra has a variety of dopamine receptor variants, most antiparkinsonian medications seem to work best when the D2 receptor form is activated.
Levodopa
Dopamine’s parent, L-dopa ((-)-3-(3,4-dihydroxyphenyl)-l-alanine or levodopa), is utilized instead since it has a lower bioavailability and more rapidly crosses the blood-brain barrier. The enzyme heterocyclic L-amino acid decarboxylase (dopa decarboxylase), which would be ubiquitous in many bodily tissues as well as the brain, converts this amino acid into dopamine after entering the brain through the use of a L-amino acid transporter (LAT). Carbidopa, a medication that does not pass the blood-brain barrier instead blocks dopa decarboxylase in peripheral tissues, is frequently used along with levodopa. The plasma half-life is lengthened, smaller doses of levodopa are efficacious, and there are less peripheral adverse effects when these two drugs are combined. Lately, an extended-release version received approval.
In the initial few years of use, levodopa produces the most beneficial effects. This might happen when levodopa dosages that were first well taken must be gradually decreased to minimize side effects. A loss of dopaminergic nigrostriatal nerve endings or another pathological event that actively engages striatal dopamine receptors may drive certain patients to become less sensitive to levodopa.
In addition to reducing mortality, levodopa improves bradykinesia and other parkinsonian symptoms. However, the medication does not treat parkinsonism, and responsiveness changes over time and begins to decline, which may indicate the disease’s development. Occasionally, variations in therapeutic outcome could be caused by when levodopa is administered. Other times, unrelated to dosage, off-periods of akinesia may cycle over the course of a few hours with on-periods of enhanced mobility, but frequently with dyskinesias (on-off phenomena). Off-periods may occasionally react to apomorphine or a more recent medication called istradefylline. A selective inhibitor of the adenosine A2A receptor, istradefylline is a caffeine derivative. Drug holidays no longer come highly suggested even if they occasionally lessen harmful effects and infrequently impact response variability. Contrarily, catechol-O-methyltransferase (COMT) inhibitors are frequently used in conjunction with levodopa to stabilize some individuals’ levodopa responsiveness.
The majority of negative effects depend on dose. Anorexia, nauseousness, and emesis are gastrointestinal adverse effects that can be lessened by taking the medication in staggered doses. Levodopa’s emetic effect normally leads to resistance after many cycles of intake.
Particularly in the beginning phases of therapy, postural hypotension is frequent. Tachycardia, asystole, and infrequently cardiac arrhythmias are further cardiac side effects. Up to 80% of patients showed dyskinesias, with choreoathetosis most frequently affecting the head and distal appendages. In some cases, chorea, ballismus, muscle twitching, repetitive movements, and tremor may be present.
Anxiety, agitation, disorientation, delusions, hallucinations, and depression are a few behavioral consequences that may occur. Those with a history of psychosis should not use levodopa.
Pramipexole
A non-ergot medication called pramipexole has a high affinity for the dopamine D3 receptor as an agonist. In cases of more severe parkinsonism, it can be used with levodopa and is useful as a monotherapy. When treating patients with renal failure, pramipexole dosage may need to be decreased. Anorexia, nausea, vomiting, postural hypotension, and dyskinesias are some of the negative consequences. Toxicities include mental problems, which are more frequent with pramipexole and ropinirole than with levodopa. Rarely with pramipexole, it’s possible to develop an uncontrollable urge to nod off. Those with active peptic ulcer disease, mental disorder, or a prior myocardial infarction should not use the medication. Yet, its capacity to detoxify hydrogen peroxide and boost neurotrophic activity in mesencephalic dopaminergic cell cultures has favorably revealed a potential neuroprotective function.
Ropinirole
Ropinirole, which is also a non-ergot, has a strong pharmacological binding for the dopamine D2 binding site. It works well as a standalone drug but can also be used with levodopa to reduce response swings. A prolonged release form can be taken once day but the standard form must be taken three times daily. Hepatic CYP1A2 is responsible for the metabolism of ropinirole, and medications that also use this isoform, such as warfarin and 1,3,7-trimethylxanthine (caffeine), may lessen the drug’s elimination. Similar side effects and warnings exist for pramipexole.
Apomorphine
Apomorphine, a powerful dopamine receptor activator, should offer patients who received optimal dopaminergic medication quick respite from akinesia off-periods around 10 minutes, but only brief reprieve within an hour or two. Pretreatment with antiemetics such trimethobenzamide for three days is required due to the severity of the nausea. Apomorphine also causes dyskinesias, hypotension, sleepiness, and sweating as adverse effects.
Rotigotine
Rotigotine is a more recent dopamine ligand that is used topically. It is hypothesized that in initial parkinsonism, it acts more gradually and continuously than oral dopamine agonists. Less is known about its effectiveness in more severe illness. Advantages and adverse reactions are comparable to those of other dopamine agonists, however reactions at the targeted site can also happen and can occasionally be severe.
Bromocriptine
Bromocriptine, an ergot compound, partially activates dopamine D2 neuronal receptors. The medication boosts dopamine neurotransmitter circuits’ physiological function, especially those engaged in extrapyramidal processes.
When treating patients who are refractory to or unable to take levodopa, bromocriptine was employed as standalone drug, in conjunction with levodopa, and with anticholinergic medications. Throughout the past, bromocriptine was frequently used to to manage Parkinson’s disease; however, the contemporary dopamine agonists have largely replaced it in this regard.
Pergolide
Another ergot derivative called pergolide directly activates both D1 and D2 receptors. Since its use has been linked to the emergence of valvular heart disease, it is not anymore commercially available in the United States despite also being extensively used for Parkinson’s disease. Yet, several nations continue to use it.
Monoamine Oxidase Inhibitors
In the neurological system, there are two distinct monoamine oxidase genotypes. Norepinephrine, serotonin, and dopamine are all metabolized by monoamine oxidase A, whereas dopamine is only metabolized by monoamine oxidase B.
At normal concentrations, selegiline (deprenyl) selectively and irreversibly inhibits monoamine oxidase B, but at larger doses, it is also known to inhibit monoamine oxidase A. Levodopa’s antiparkinsonian impact is enhanced and prolonged by selegiline, which allows for a decrease in levodopa dosage. Selegiline also slows the degradation of dopamine. Moreover, this lessens minor wearing-off or on-off occurrences. As a result, it serves as an adjuvant treatment for individuals whose responsiveness to levodopa is waning or variable. Desmethylselegiline, a substance that may have neuroprotective properties, and amphetamine are produced as a result of selegiline’s hepatic metabolism.
Another monoamine oxidase B inhibitor is rasagiline. Rasagiline has been utilized both independently and in tandem with levodopa to treat early clinical parkinsonism. This medication has been demonstrated to be more successful than selegiline at averting MPTP-induced parkinsonism.
A comparable MAO-B-selective inhibitor that has finally acquired approval is safinamide. It is employed to lessen off-periods in individuals with wearing-off effect or on-off phenomena and responsive variability in subjects receiving carbidopa and levodopa. Safinamide doesn’t seem to be effective when used alone.
Monoamine oxidase inhibitors can have undesirable side effects and interactions, such as sleeplessness, mood swings, dyskinesias, digestive problems, and low blood pressure. Irritation, disorientation, and even death have been reported when these medications are used with meperidine. When administered in conjunction with serotonin selective reuptake inhibitors (SSRIs), selegiline has been linked to the serotonin syndrome.
Catechol-O-methyltransferase Inhibitors
The COMT enzyme, which is present in both the central and peripheral nervous systems and transforms levodopa to 3-O-methyldopa (3-OMD), is inhibited by entacapone and tolcapone. Levodopa responsiveness is negatively correlated with higher plasma levels of 3-OMD, in part since the substance competes with levodopa for facilitated diffusion into the brain. Entacapone solely has peripheral effects. An equivalent COMT inhibitor opicapone has just received approval in the USA and Europe.
Levodopa-carbidopa therapy is supplemented with catechol-O-methyltransferase inhibitors to reduce fluctuations, enhance responsiveness, and lengthen on-time effects. Entacapone is taken five times per day while tolcapone is administered thrice. Levodopa, carbidopa, and entacapone are available in a formulation that streamlines the medication schedule.
Negative reactions attributed partly to elevated levels of levodopa comprise dyskinesias, gastrointestinal distress, and postural hypotension. Within the initial few times after starting a COMT inhibitor regimen, levodopa dosage decreases can indeed be necessary. Sleep disturbances and urine that has an orange tint are some other negative effects. For usage in the United States, tolcapone requires constant monitoring of liver function measurements and written patient consent due to its increased liver enzyme levels and history of acute hepatic impairment.
Amantadine
Through unknown pathways, amantadine (1-adamantylamine or 1-aminoadamantane) improves dopaminergic neurotransmission. These mechanisms could entail enhancing dopamine biosynthesis or release or regulating dopamine recapture. The medication also inhibits muscarinic receptors. Amantadine may reduce rigidity, tremor, and bradykinesia, but its effects often last only a few weeks. Amantadine has antiviral properties like its closely related adamantane derivative rimantadine where they both target the M2 proton channel of influenza A virus.
Severe toxic psychosis, restlessness, irritability, sleeplessness, disorientation, hallucinations, and anxiety are some behavioral consequences. The netlike pattern of reddish-blue skin discoloration livedo reticularis is one typical dermatologic adverse reaction. Gastrointestinal issues, urine retention, and postural hypotension are examples of other side effects. The peripheral edema side effect of amantadine is shown to be easily addressed with diuretics.
Acetylcholine-Blocking (Antimuscarinic) Drugs
Antimuscarinic xenobiotics like ophenadrine, biperiden, and benztropine work by blocking muscarinic receptors to lessen the excitatory effects of cholinergic neurons on cells in the striatum.
These medications may reduce the rigidity and tremor associated with parkinsonism, but they have little impact on bradykinesia. In addition to treating parkinsonism, they also lessen the transient extrapyramidal symptoms brought on by antipsychotic medications. Drowsiness, inattentiveness, disorientation, psychosis, and hallucinations are all symptoms of CNS overdose. Drugs that are similar to atropine frequently have peripheral withdrawal symptoms. These substances aggravate tardive dyskinesias induced on by protracted antipsychotic medication exposure.
Drug Therapy for Nonmotor Manifestations
To alleviate the psychiatric problems of advanced parkinsonism, additional medications could be required. A 5-HT2A (5-hydroxytryptamine or serotonin) inverse agonist called pimavanserin has been authorized specifically for psychosis linked to Parkinsonism. Atypical antipsychotics may very well be helpful for comparable indications.
Donepezil, rivastigmine, and memantine can all have a beneficial effect on those with cognitive deterioration. Antidepressants or anxiolytic medications have been found to help patients with mood and affective problems, while individuals who have excessive daytime sleepiness can benefit from modafinil‘s CNS stimulant activity. Appropriate symptomatic therapy is recommended for people who have bladder and bowel issues.
Deep Brain Stimulation
In principle, functional, reversible lesions caused by high-frequency deep brain stimulation have supplanted invasive surgical methods for parkinsonism because they have a reduced morbidity. For the therapy of the clinical irregularities or dyskinesias appearing in milder parkinsonism, activation of the globus pallidus or subthalamic nucleus with an implanted electrode and stimulator has produced favorable results. Individuals with secondary or idiosyncratic parkinsonism, dementia, or inability to react to dopaminergic treatment should avoid undergoing such interventions. Patients receiving deep brain stimulation can frequently have their antiparkinsonian dosage decreased, which may aid to lessen the harmful dose-related pharmaceutical effects.
Neuroprotective Therapy
Antioxidants, antiapoptotic agents, glutamate antagonists, glial-derived neurotrophic factor, and anti-inflammatory medications are some of the substances that have been studied as potential neuroprotective agents to halt disease development. However, none of these substances have been demonstrated to be efficient in this situation, thus their usage for therapeutic purposes is not advised at this time.
Despite early promises to the contrary, coenzyme Q10, creatine, pramipexole, and pioglitazone have not been found to be beneficial. Rasagiline may have a protective effect, as was previously discussed. There is ongoing exploration of α-synuclein immunization in both active and passive forms.
Gene Therapy
Gene therapy for Parkinson’s disease has undergone a number of phase 1 (safety) or phase 2 trials in the USA. Adeno-associated virus type 2 was used in every trial as the genetic carrier and was delivered into the striatum. The genes were GAD, AADC, and neurturin.
The genes for glutamic acid decarboxylase (GAD) are incorporated into the subthalamic nucleus to expedite the production of γ-aminobutyric acid (GABA), an inhibitory neurotransmitter that alleviates muscle stiffness in Parkinson’s. Those of aromatic acid decarboxylase’s (AADC) are infused into the putamen to enhance metabolic activity of levodopa to dopamine. Finally, genes for neurturin, a growth factor, are also infused into the putamen in hopes of improving the survival of dopaminergic neurons. The data indicated efficacy and all the medicines were declared safe.
The results of a phase 2 trial on the GAD gene are promising, while those for neurturin injections into the putamen and substantia nigra were unsatisfactory. A phase 2 AADC trial is anticipated. ProSavin is a lentiviral vector-based gene therapy with three genes (decarboxylase, tyrosine hydroxylase, and GTP-cyclohydrolase 1) intended to restore local and continuous dopamine production in patients with advanced Parkinson’s disease. The results of a European study involving bilateral intrastriatal delivery of ProSavin have also been encouraging.
Origin of the Disease’s Name
The condition was first described as “paralysis agitans” by English physician James Parkinson, FGS, in his 1817 publication An Essay on the Shaking Palsy. Jean-Martin Charcot, the father of modern neurology, eventually dubbed this ailment as Parkinson’s disease. Public awareness activities include the usage of a red tulip as the disease symbol and World Parkinson’s Day, which is observed on April 11—James Parkinson’s birthday.
Subscribe
to get our
LATEST NEWS
Related Posts

Chronic & Debilitating Diseases
Renopathology Tipping Point: Deciphering the Molecular Code of Stage 2 Chronic Kidney Disease
The molecular events of Stage 2 CKD, from inflammation to lipid metabolism, offer insights for diagnosis and treatment.
Chronic & Debilitating Diseases
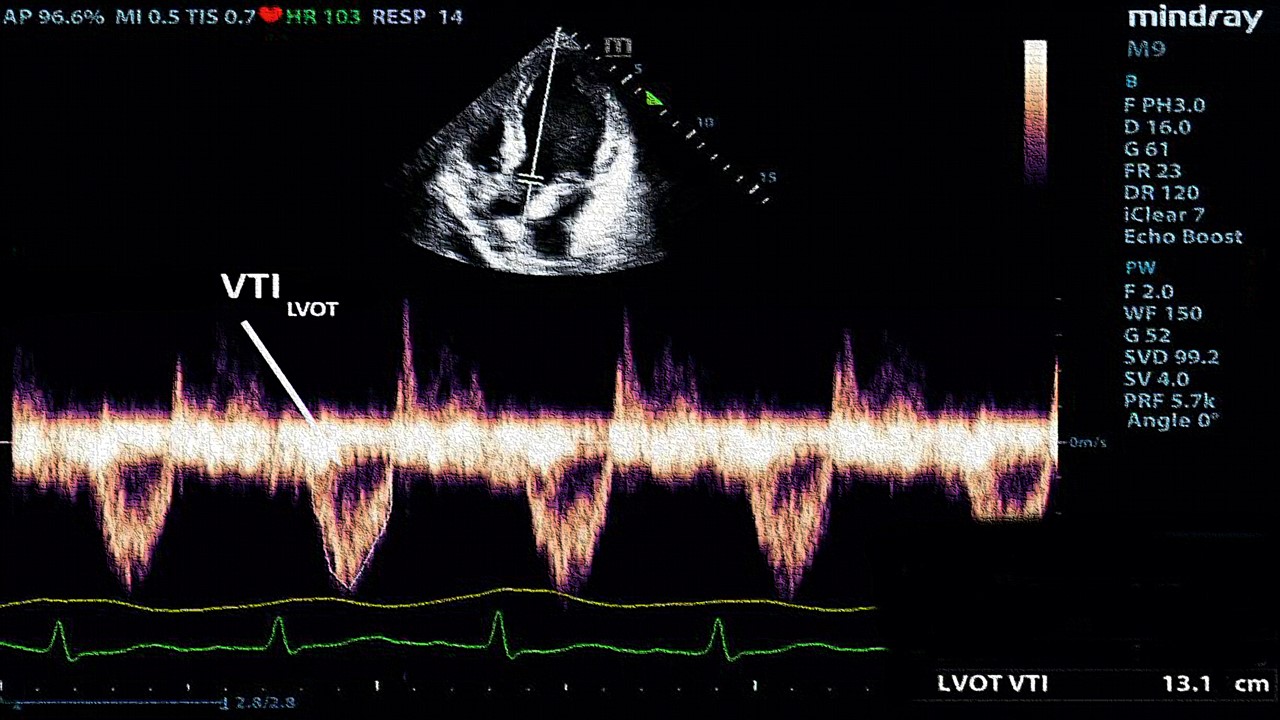
A New Lens on Shock: Hemodynamic Insights Through Critical Care Ultrasound
CCU has transformed the hemodynamic assessment of shock, delivering a reliable, reproducible, and non-invasive tool for ICU clinicians.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.
Designing Better Sugar Stoppers: Engineering Selective α-Glucosidase Inhibitors via Fragment-Based Dynamic Chemistry
One of the most pressing challenges in anti-diabetic therapy is reducing the unpleasant and often debilitating gastrointestinal side effects that accompany α-amylase inhibition.