Cancer has long been a disease of genetic dysregulation, where mutations and aberrant gene expression drive uncontrolled proliferation. Traditional therapies—chemotherapy, radiation, and even many targeted drugs—act broadly, often with significant collateral damage. RNA-based therapeutics, including small interfering RNA (siRNA) and antisense oligonucleotides (ASOs), represent a paradigm shift, offering precision targeting at the molecular level. These molecules can selectively silence disease-causing genes, offering a new frontier in oncology where treatment is as precise as the genetic defects themselves. The potential to disrupt oncogenic pathways without harming healthy tissue positions RNA drugs as one of the most promising advancements in cancer therapy.
The Molecular Scalpel: How RNA Therapeutics Target Cancer
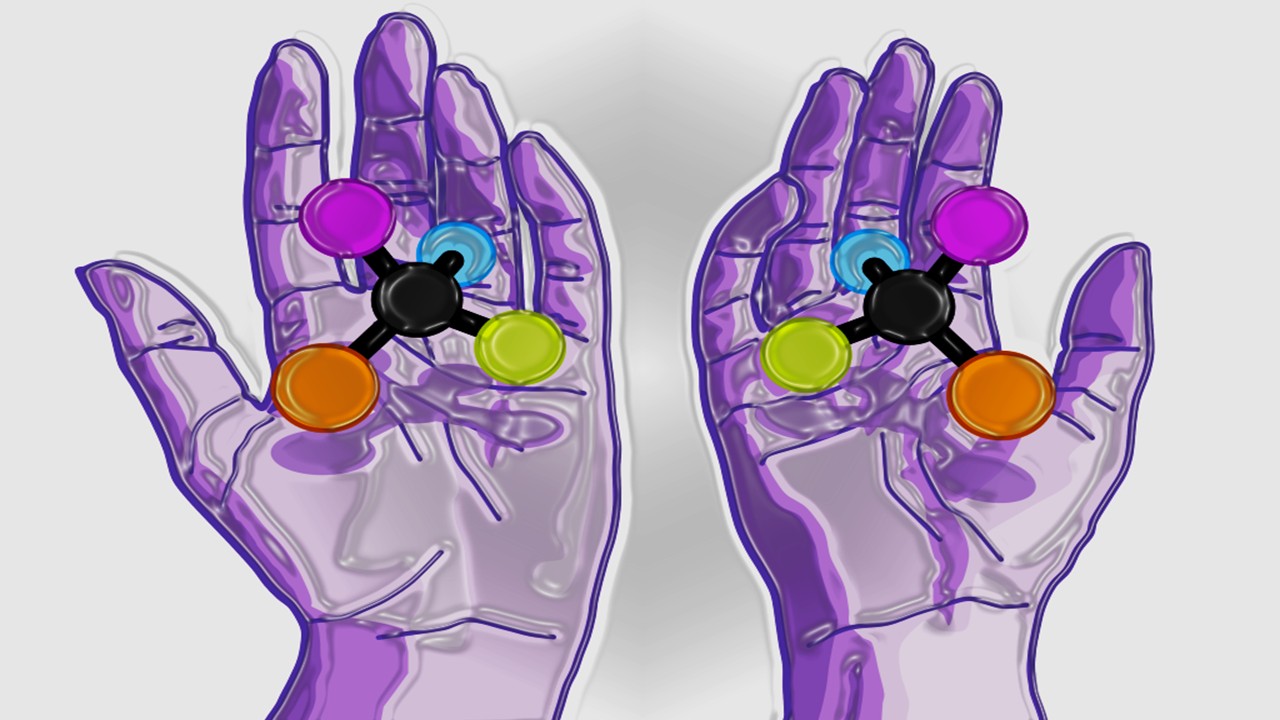
RNA interference (RNAi) and antisense technology exploit the cell’s own machinery to suppress harmful gene expression. siRNA molecules guide the RNA-induced silencing complex (RISC) to degrade specific messenger RNA (mRNA), preventing translation into pathogenic proteins. ASOs, on the other hand, bind directly to target RNA, either blocking ribosomal access or triggering enzymatic degradation. Both strategies enable the selective knockdown of oncogenes, fusion transcripts, or resistance factors that drive tumor survival.
The specificity of RNA-based drugs is unprecedented. Unlike small-molecule inhibitors, which often interact with multiple unintended targets, siRNA and ASOs are designed with exact complementarity to their RNA targets. This reduces off-target effects, a major limitation of conventional therapies. Computational algorithms optimize sequence selection to maximize silencing efficiency while minimizing immune activation or unintended RNA interactions. The result is a therapeutic agent that functions like a molecular scalpel, excising only the defective genetic instructions fueling malignancy.
Delivery remains the most formidable challenge. Naked RNA is rapidly degraded by nucleases and poorly internalized by cells. Lipid nanoparticles (LNPs), conjugation to targeting ligands, and chemical modifications such as phosphorothioate backbones enhance stability and cellular uptake. Recent advances in LNP formulations, initially validated in mRNA vaccines, now enable efficient siRNA delivery to tumors. Researchers emphasize that refining these delivery systems is critical for expanding the clinical applicability of RNA drugs beyond liver-centric targets.
The modularity of RNA therapeutics allows rapid adaptation to evolving tumors. Resistance mutations that render small-molecule drugs ineffective often leave RNA targets intact. If a tumor escapes therapy by upregulating an alternative pathway, new siRNA or ASO sequences can be designed within weeks, outpacing the slow development cycles of traditional pharmaceuticals. This agility is particularly valuable in cancers with high mutational burdens, such as melanoma or lung adenocarcinoma.
Ultimately, RNA-based drugs exploit the fundamental language of biology to rewrite cancerous programs. By directly intercepting the flow of genetic information, they offer a level of intervention that was previously unimaginable in oncology.
Oncogene Addiction: Exploiting Cancer’s Genetic Vulnerabilities
Many cancers exhibit oncogene addiction—a dependency on specific overactive genes for survival. RNA therapeutics are uniquely suited to exploit this Achilles’ heel by silencing these critical drivers. For example, MYC, KRAS, and BCL-2, long considered “undruggable” by conventional means, are now being targeted with siRNA and ASOs in preclinical and clinical studies.
MYC, a master regulator of proliferation, is amplified in numerous cancers. Small-molecule inhibitors have struggled to disrupt MYC function due to its lack of enzymatic activity and pervasive protein-protein interactions. MYC-targeting siRNAs, delivered via LNPs, have shown remarkable efficacy in reducing tumor growth in hepatocellular carcinoma models without systemic toxicity. Researchers suggest that this approach could be transformative for MYC-driven malignancies, which are notoriously aggressive and treatment-resistant.
KRAS mutations, prevalent in pancreatic, colorectal, and lung cancers, have eluded direct inhibition for decades. While recent covalent inhibitors target specific KRAS variants like G12C, many mutations remain untouchable. Allele-specific ASOs that selectively degrade mutant KRAS mRNA while sparing the wild-type transcript are in development. Early data indicate tumor regression in models harboring G12D and G12V mutations, offering hope for patients with these historically fatal alterations.
BCL-2, an anti-apoptotic protein overexpressed in leukemias and lymphomas, is another prime target. Venetoclax, a small-molecule BCL-2 inhibitor, has demonstrated efficacy but faces resistance mechanisms. BCL-2-directed siRNAs could circumvent these issues by preventing protein synthesis altogether. Combining RNA therapeutics with existing inhibitors may further enhance tumor cell killing while delaying resistance.
The concept of synthetic lethality also applies to RNA drugs. Silencing a gene that is nonessential in normal cells but critical in tumors with specific mutations could yield highly selective therapies. PARP inhibitors exemplify this principle in BRCA-mutated cancers; analogous RNA-based strategies are being explored for other genetic contexts. By focusing on cancer’s genetic dependencies, RNA therapeutics promise to expand the roster of actionable targets beyond the reach of conventional drugs.
Overcoming Resistance: RNA Drugs in the Arms Race Against Tumors
Cancer’s ability to evolve resistance is a major therapeutic hurdle. RNA-based drugs offer several advantages in this perpetual arms race. Unlike kinase inhibitors, which often succumb to single-point mutations in their binding sites, siRNA and ASOs target mRNA sequences that are less prone to mutation without disrupting protein function.
One strategy involves simultaneously targeting multiple nodes in a resistance pathway. For instance, tumors resistant to EGFR inhibitors frequently upregulate bypass signaling through MET or AXL. Combinatorial siRNA cocktails silencing these parallel effectors can restore sensitivity. Researchers note that such multi-target approaches are more feasible with RNA drugs than with small molecules, where polypharmacology risks intolerable toxicity.
Epigenetic plasticity, another resistance mechanism, allows tumors to switch transcriptional programs in response to therapy. RNA therapeutics can target the epigenetic machinery itself—such as EZH2 or DNMTs—or downstream effectors that maintain the resistant state. In glioblastoma, where tumor cells adopt a mesenchymal phenotype to evade treatment, ASOs against key transcription factors like STAT3 have reversed this transition in preclinical models.
The immune microenvironment also plays a role in resistance. Tumors often upregulate checkpoint ligands like PD-L1 or immunosuppressive cytokines to evade T-cell attack. Local delivery of siRNA against these factors, combined with checkpoint blockade, has enhanced antitumor immunity in syngeneic models. Unlike antibody-based therapies, RNA drugs can transiently modulate the immune landscape without inducing chronic immune-related adverse events.
Finally, RNA therapeutics can address the root of resistance: cancer stem cells (CSCs). These therapy-resistant progenitors often rely on unique survival pathways, such as Wnt/β-catenin or Notch signaling. CSC-specific siRNAs, conjugated to antibodies against stem cell markers, have shown promise in eradicating this recalcitrant population in triple-negative breast cancer. By attacking resistance at multiple levels, RNA drugs could turn the tide in the battle against adaptive tumors.
Delivery Breakthroughs: Getting RNA Drugs Where They Need to Go
The efficacy of RNA therapeutics hinges on delivery. Without robust systems to transport these molecules into target cells, even the most potent sequences are useless. Recent innovations in nanotechnology, bioconjugation, and formulation science are overcoming these barriers, bringing RNA drugs closer to widespread clinical use.
Liver-targeted delivery is the most advanced, leveraging the natural tropism of LNPs and GalNAc-conjugated siRNAs for hepatocytes. This success has spurred efforts to replicate such precision in other tissues. Tumor-specific ligands, such as antibodies against EGFR or HER2, are being conjugated to RNA carriers to direct them to cancer cells. In prostate cancer, PSMA-targeted LNPs have delivered siRNAs selectively to metastatic lesions, sparing healthy tissue.
Stimuli-responsive nanoparticles add another layer of control. pH-sensitive carriers release their payload in the acidic tumor microenvironment, while light- or ultrasound-activated systems enable spatiotemporal precision. These approaches minimize off-target silencing and could be particularly valuable in cancers with sensitive adjacent structures, such as brain or pancreatic tumors.
Exosomes, naturally occurring nanovesicles, are emerging as biocompatible RNA carriers. Tumor-derived exosomes have inherent homing capabilities, efficiently delivering siRNA to their cell of origin. Bioengineered exosomes with enhanced loading capacity and targeting moieties are in development, offering a potentially universal delivery platform.
Local delivery routes—intratumoral, intraperitoneal, or inhaled—avoid systemic exposure altogether. In ovarian cancer, intraperitoneal siRNA administration has achieved robust tumor penetration with minimal hepatic sequestration. For lung cancers, nebulized RNA formulations could provide direct access to malignant lesions while bypassing the circulation.
The future of RNA delivery lies in modular systems that can be tailored to diverse cancers. As these technologies mature, the therapeutic window for RNA drugs will expand, unlocking their full potential in oncology.
Beyond Silencing: The Expanding Arsenal of RNA Therapeutics
While gene silencing dominates current RNA therapeutic strategies, emerging modalities are broadening the scope of what these molecules can achieve. RNA aptamers, mRNA vaccines, and CRISPR-based RNA editors are adding new dimensions to cancer treatment, each with unique advantages.
RNA aptamers—structured oligonucleotides that bind proteins with high affinity—can antagonize oncogenic pathways or deliver toxins selectively to tumors. A PDGF-binding aptamer has shown anti-angiogenic effects in glioblastoma, complementing traditional anti-VEGF therapies. Unlike antibodies, aptamers are chemically synthesized, enabling rapid optimization and lower production costs.
Personalized mRNA vaccines train the immune system to recognize tumor neoantigens. While most advanced in melanoma, this approach is being tested in other malignancies with high mutational loads. Intranodal delivery of mRNA encoding patient-specific mutations has induced robust T-cell responses in early trials, suggesting a viable alternative to cumbersome cell therapies.
CRISPR-Cas13, an RNA-targeting counterpart to DNA-editing Cas9, introduces the possibility of transcriptome engineering. Unlike permanent DNA edits, transient RNA manipulation reduces off-target risks while allowing dose titration. Cas13 systems programmed to cleave oncogenic RNAs could offer a “tunable” form of gene therapy, particularly for fusion-driven cancers like Ewing sarcoma.
RNA base editors, which convert one nucleotide to another without cutting the transcript, enable more subtle interventions. Correcting a single pathogenic mutation in an otherwise functional mRNA could restore normal protein function—an approach under investigation for TP53-mutant cancers.
The versatility of RNA as both a drug and a drug target makes it a uniquely powerful platform. As these technologies converge, the line between gene therapy and pharmacotherapy will blur, giving rise to a new class of precision oncology tools.
Clinical Frontiers: RNA Therapeutics in Human Trials
The translational pipeline for RNA-based cancer therapies is rapidly expanding. From early-phase safety studies to randomized controlled trials, these interventions are demonstrating tangible benefits across diverse malignancies.
Inotersen, an ASO approved for hereditary transthyretin amyloidosis, has inspired oncology applications. Similar chemistry is being tested in AML, where ASOs against the fusion oncogene RUNX1-ETO have reduced leukemia burden in preclinical models. Researchers highlight that repurposing proven RNA platforms accelerates oncology development, reducing the time from bench to bedside.
The first siRNA drug for cancer, patisiran (originally for polyneuropathy), is being evaluated in ATTR amyloidosis with cardiac involvement, a condition with malignant parallels in protein aggregation. Lessons from its use—particularly in managing infusion-related reactions—inform safer administration protocols for oncologic siRNAs.
Solid tumors pose greater delivery challenges, but progress is being made. A phase I trial of EphA2-targeting siRNA in advanced cancers showed tumor regression in some patients with acceptable toxicity. Imaging studies confirmed nanoparticle accumulation in metastatic lesions, validating the delivery approach.
Combination strategies are also entering the clinic. An siRNA suppressing the immunosuppressive cytokine TGF-β is being tested with PD-1 blockade in melanoma, based on preclinical synergy. Early signals suggest enhanced T-cell infiltration and prolonged responses compared to checkpoint inhibition alone.
Pediatric cancers, often driven by fusion oncoproteins, are another focus. An ASO targeting the EWS-FLI1 fusion in Ewing sarcoma has entered clinical testing, offering hope for a disease with limited targeted options. The ability to design RNA drugs against unique breakpoints makes them ideal for such genetically defined pediatric malignancies.
As these trials mature, they will define the clinical niches where RNA therapeutics outperform existing modalities. The coming decade will likely see the first approvals of RNA drugs for cancer, marking a new era in precision oncology.
The Future of RNA Medicine in Oncology
The trajectory of RNA-based cancer therapy points toward increasingly sophisticated interventions. Next-generation chemistries, such as bicyclic RNAs and gamma-modified backbones, promise enhanced potency and duration of effect. These advances could reduce dosing frequency, improving patient compliance and cost-effectiveness.
Tissue-specific delivery will expand beyond the liver. Advances in capsid engineering for viral vectors and novel nanoparticle formulations are enabling RNA drug delivery to the brain, lungs, and other historically challenging sites. This could revolutionize treatment for glioblastoma, small cell lung cancer, and other recalcitrant malignancies.
Integration with diagnostics will enable dynamic therapy adjustments. Liquid biopsies detecting emerging resistance mutations could trigger the administration of tailored RNA cocktails, creating a closed-loop therapeutic system. Such real-time adaptation would render cancer a chronically manageable condition rather than a relentlessly progressive disease.
The democratization of RNA drug design is another anticipated shift. As computational tools for siRNA and ASO design become more accessible, academic centers and smaller biotechs will contribute to the therapeutic arsenal. This decentralized innovation model could accelerate discovery for rare cancers underserved by large pharma.
Ultimately, RNA therapeutics represent more than just a new drug class—they embody a fundamental shift in how we intervene in disease. By operating at the level of genetic information flow, they offer a precision and adaptability unmatched by traditional pharmacology. As delivery hurdles fall and clinical validation grows, RNA drugs may well become the cornerstone of 21st-century oncology.
Rewriting the Rules of Cancer Treatment
RNA-based therapeutics are poised to redefine cancer therapy, offering unparalleled specificity, adaptability, and a growing repertoire of mechanisms. From silencing once-“undruggable” oncogenes to dynamically countering resistance, these molecules exploit the very essence of cancer’s genetic derangement.
While challenges remain—particularly in delivery and manufacturing—the pace of innovation is staggering. What began as a scientific curiosity in gene silencing has matured into a robust therapeutic platform with life-saving potential. The coming years will see RNA drugs transition from promising outliers to mainstream oncology tools, offering new hope for patients with limited options.
In the grand narrative of cancer treatment, RNA therapeutics represent not just another chapter, but a new volume altogether—one where the language of life itself becomes the medium of cure.
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES

Subscribe
to get our
LATEST NEWS
Related Posts

Medicinal Chemistry & Pharmacology
Polarity Alchemy: Strategic Charge Manipulation in Contemporary Drug Design
The future promises tunable therapies with polarity adjustable by light, magnetic fields, or bioorthogonal triggers.

Medicinal Chemistry & Pharmacology
Metabolic Saboteurs: Precision Drug Design Against Pathological Pathways
The next frontier in precision medicine lies in drugs that surgically disrupt disease-specific metabolic pathways and recalcitrant enzymes.
Read More Articles
Chemical Gale: How Wind Energy is Reshaping Industrial Manufacturing
The integration of wind energy into chemical manufacturing constitutes a fundamental reimagining of process chemistry.
Algorithmic Trials: How Decision Theory is Reshaping Decentralized Clinical Research
Decision theory offers a robust mathematical framework to design trials that enhance efficiency, uphold ethical standards, and better reflect the complexities of real-world therapeutic contexts.