Ischemic heart disease (IHD) stands as the leading cause of death worldwide, despite major advances in diagnostic and therapeutic strategies. Atherosclerotic disease, which affects the epicardial arteries, is the well-recognized primary cause of IHD. However, a significant percentage of patients experiencing ST-elevation myocardial infarction (STEMI) exhibit no discernible coronary artery disease (CAD) upon angiography, raising the possibility of alternative underlying mechanisms. Acute myocardial injury (AMI) is typically diagnosed using a combination of symptoms and elevated cardiac biomarkers such as troponin, as defined by the Fourth Universal Definition of Myocardial Infarction.
In cases where coronary plaques—representing 50% or more stenosis of the epicardial arteries—are excluded, and other conditions such as pulmonary embolism or myocarditis are ruled out, clinicians apply the diagnosis of myocardial infarction with non-obstructive coronary artery disease (MINOCA). Despite its first mention over 75 years ago, MINOCA remains an elusive and often misunderstood condition. It has been noted in clinical studies to represent anywhere from 5% to 15% of all AMI cases, depending on the population studied. The presence of MINOCA complicates our understanding of ischemic heart disease, as it challenges the long-standing assumption that coronary artery blockages are the sole drivers of myocardial infarction.
INOCA and Its Unique Risk Profile
In addition to MINOCA, there exists another condition known as ischemia with non-obstructive coronary arteries (INOCA). While the latter is more prevalent in women and associated with a higher risk of adverse cardiovascular events, its key differentiator from MINOCA lies in the absence of acute myocardial infarction. In INOCA, patients experience episodes of ischemia without significant coronary artery blockages, a condition that has been linked to coronary microvascular dysfunction (CMD) and is often associated with conditions such as heart failure with preserved ejection fraction (HFpEF) and stroke.
The risk factors for MINOCA and INOCA differ notably. For MINOCA, predisposing factors include hypertension, psychological stress, younger age, and platelet disorders. INOCA, by contrast, is more common in older individuals and is typically associated with traditional cardiovascular risk factors like dyslipidemia, diabetes, and smoking. This divergence in risk profiles further underscores the complexity of diagnosing and managing these two conditions.
Pathophysiology of Coronary Blood Flow
To understand the underlying mechanisms of MINOCA, one must first consider the physiology of the coronary arteries. The coronary arterial system is a complex network that includes both large epicardial arteries and smaller arterioles. While the epicardial arteries offer minimal resistance to blood flow, the arterioles, pre-arterioles, and capillaries—which make up the coronary microcirculation—account for the majority of resistance within the heart’s circulatory system. In healthy individuals, coronary blood flow (CBF) is tightly regulated by various mechanisms, including endothelial, neurohumoral, nervous, metabolic, and myogenic controls.
Endothelial cells play a critical role in the regulation of vasomotor activity by releasing vasoactive substances such as nitric oxide (NO) and endothelin-1 (ET-1). A delicate balance between these substances ensures proper dilation and constriction of the coronary arteries. However, oxidative stress and chronic inflammation can disrupt this balance, reducing NO availability and increasing the vasoconstrictive effects of ET-1. This shift is further exacerbated by the transformation of NO into reactive oxygen species (ROS), leading to endothelial dysfunction.
Beyond the endothelium, the nervous system also influences coronary blood flow. The parasympathetic nervous system, through acetylcholine production, promotes vasodilation, while the sympathetic system—depending on which receptors are activated—can cause either vasoconstriction or vasodilation. Myogenic mechanisms allow the coronary arteries to self-regulate, maintaining consistent blood flow despite fluctuations in blood pressure. Additionally, metabolic regulation, influenced by factors such as adenosine and ATP, plays a crucial role in adjusting blood flow based on the oxygen demands of myocardial tissue.
Pathophysiological Mechanisms Behind MINOCA
MINOCA can be attributed to both atherosclerotic and non-atherosclerotic mechanisms. The former includes plaque disruption, a process that may involve plaque rupture, erosion, or calcification. This disruption often leads to thrombus formation, which can result in myocardial infarction, even in the absence of significant coronary artery blockages. Intravascular imaging has revealed plaque disruptions in approximately one-third of MINOCA patients, underscoring the role of subtle atherosclerotic changes in this condition.
Non-atherosclerotic mechanisms encompass a broader range of causes, including epicardial coronary vasospasm, CMD, coronary embolism or thrombosis, spontaneous coronary artery dissection, and imbalances between oxygen supply and demand. Vasospasm, triggered by smooth muscle hyperreactivity, can be induced by both endogenous factors (such as hormones) and exogenous substances (like cocaine). In patients undergoing provocative testing, inducible vasospasm has been observed in over 25% of cases, suggesting that this is a significant contributor to MINOCA. Coronary thrombosis or embolism, on the other hand, may be caused by inherited or acquired thrombotic disorders, with emboli lodging in the coronary microcirculation and causing localized ischemia.
Spontaneous coronary artery dissection (SCAD) represents another non-atherosclerotic cause of MINOCA, particularly among younger women. SCAD is often linked to hormonal changes, pregnancy, and delivery, and it can occur without any evidence of atherosclerosis. Interestingly, SCAD-related dissections often affect the microvasculature and may not be visible on routine angiography, further complicating diagnosis. Supply-demand mismatch, a hallmark of type II myocardial infarction, can also lead to MINOCA. This mismatch is typically associated with arrhythmias, hypotension, or hypoxia, and in many cases, patients with MINOCA exhibit no significant CAD, suggesting that their condition arises from these non-obstructive mechanisms.
The Hidden Role of Coronary Microvascular Dysfunction in MINOCA
CMD plays an underappreciated role in Myocardial Infarction with Non-Obstructive Coronary Arteries (MINOCA), affecting nearly half of these patients, particularly women. These microvessels—often invisible on traditional angiograms—are crucial in controlling blood flow to the heart. When they malfunction, the consequences can range from chronic chest pain to full-blown myocardial infarction, even in the absence of major blockages. CMD results from structural changes like vessel narrowing and functional problems like impaired endothelial responses. These abnormalities disrupt blood flow regulation, leading to ischemia and potentially heart muscle damage.
Impaired nitric oxide production, microvascular spasms, and thickened vessel walls all contribute to this dysfunction. The lack of visible blockages can make CMD elusive to diagnose, yet measuring microvascular resistance (IMR) provides insight into its severity. As more is understood about CMD’s role in MINOCA, it becomes clear that its contribution to patient outcomes may be as significant as larger vessel disease, yet much harder to detect.
Unraveling the Complex Web of CMD: Inflammation, Stress, and Thrombosis
CMD is not just a mechanical issue—it involves a complex interplay of factors, including inflammation, stress, and thromboembolic phenomena. Myocarditis, for instance, inflames the heart tissue and compresses microvessels, leading to ischemia. Viral infections, such as parvovirus B19, are often at the heart of this inflammation. Moreover, CMD’s link with stress-related triggers is supported by the observed increase in MINOCA cases during high-stress periods, hinting that psychological and physiological stressors can directly impact coronary microcirculation.
Thrombosis is another player in this intricate system. Microvascular obstruction can occur when small clots or plaque debris obstruct blood flow in the smallest vessels. In patients with underlying thrombophilic conditions like Factor V Leiden or antiphospholipid syndrome, the likelihood of microvascular clots rises, especially in young women with unexplained MINOCA. These findings underscore CMD’s multifaceted nature, where microvascular health is influenced by a cascade of events that transcend simple vascular blockages, suggesting that targeted diagnostic and therapeutic strategies will be crucial in improving outcomes.
MINOCA and Coronary Microvascular Dysfunction: The Genetic Susceptibility
The genetic predisposition to IHD and CMD is increasingly becoming a focus of research, with genetic susceptibility thought to play a crucial role in these conditions. More than 50% of IHD susceptibility is believed to stem from genetic variants, particularly single-nucleotide polymorphisms (SNPs). These genetic differences can influence proteins that regulate CBF, leading to an increased risk of CMD and, subsequently, MINOCA. Some genetic variants even confer protective properties, potentially reducing susceptibility to ischemia.
Genome-wide association studies (GWAS) have pinpointed key loci, such as the CDKN2B-AS1 gene on chromosome 9p21, which affect vascular function and contribute to CMD. The interactions between these loci, inflammatory pathways, and proteins such as vascular endothelial growth factor-A (VEGF-A) underscore the genetic complexity of MINOCA. Other studies have identified polymorphisms in genes like HMOX1 and ET-1, which may influence endothelial function and vascular response to stress. As our understanding of these pathways deepens, the potential for targeted therapies based on a patient’s genetic profile grows, offering hope for more personalized treatment strategies for CMD and MINOCA in the future.
Diagnostic and Therapeutic Approaches to MINOCA
Diagnosing MINOCA requires a careful and methodical approach, given the absence of significant coronary artery blockages. Clinicians must first rule out alternative causes of myocardial injury, such as myocarditis, pulmonary embolism, or stress-induced cardiomyopathy (Takotsubo syndrome). Advanced imaging techniques, including intravascular ultrasound (IVUS) and optical coherence tomography (OCT), can provide additional insights into the condition by detecting subtle plaque disruptions or microvascular abnormalities.
Once a diagnosis of MINOCA has been established, treatment must be tailored to the underlying cause. In cases where vasospasm is suspected, calcium channel blockers or nitrates may be prescribed to reduce smooth muscle hyperreactivity. Antiplatelet therapy, such as aspirin or clopidogrel, is recommended for patients with suspected thrombotic or embolic causes. In patients with CMD, therapies aimed at improving microvascular function—such as angiotensin-converting enzyme inhibitors (ACEIs) or statins—may be considered. However, given the heterogeneity of the condition, individualized treatment plans are essential for achieving optimal outcomes.
Current Pharmacological Approaches
From a pharmacological standpoint, managing MINOCA is challenging due to its diverse underlying mechanisms. Antiplatelet agents, particularly aspirin, remain a cornerstone of therapy in cases involving suspected plaque disruption or thrombus formation. However, for patients with vasospastic angina or coronary microvascular dysfunction, calcium channel blockers and nitrates are often employed to improve blood flow and reduce vasospasm. Beta-blockers, while effective in traditional myocardial infarction, may be less beneficial in MINOCA patients, particularly in those with CMD, where microvascular dysfunction plays a more prominent role.
Emerging therapies targeting endothelial dysfunction, such as NO donors and ET-1 antagonists, are also being explored as potential treatment options for patients with CMD. These agents aim to restore the delicate balance between vasodilation and vasoconstriction in the coronary microcirculation, potentially improving outcomes for patients with MINOCA and INOCA alike.
As our understanding of MINOCA evolves, so too does the potential for more precise and personalized treatment strategies. By continuing to unravel the complexities of this enigmatic condition, researchers and clinicians can hope to improve the lives of the many patients who suffer from ischemic heart disease in its more elusive forms.
Bridging Pharmacology, Diagnostics, and Genomics in Modern Cardiology
The intricate relationship between MINOCA (Myocardial Infarction with Non-Obstructive Coronary Arteries) and INOCA (Ischemia with Non-Obstructive Coronary Arteries) highlights the multifaceted nature of ischemic heart disease (IHD). Both conditions challenge traditional diagnostic frameworks, as they involve microvascular dysfunction rather than obstructive lesions in coronary arteries. The exploration of pharmacological approaches is crucial for managing these patients, particularly in light of emerging treatments aimed at alleviating symptoms and improving coronary flow.
Moreover, advancements in genomics provide invaluable insights into the genetic underpinnings of CMD and IHD. The identification of specific SNPs and genetic variants that influence disease susceptibility allows for more precise diagnostics and personalized treatment strategies. By integrating pharmacological interventions with genetic profiling, healthcare providers can better predict outcomes and tailor therapies to individual patients, ultimately enhancing the management of MINOCA and INOCA. This holistic approach underscores the importance of interdisciplinary collaboration in addressing the complexities of cardiovascular health and advancing patient care.
Study DOI: https://doi.org/10.3390/jcm12103586
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES
Register your interest [here] at Proventa International’s Clinical Operations and Clinical Trials Supply Chain Strategy Meeting this 14th of November 2024 at Le Meridien Boston Cambridge, Massachusetts, USA to engage with thought leaders and like-minded peers on the latest developments in the clinical space and regulatory affairs.

Subscribe
to get our
LATEST NEWS
Related Posts

Chronic & Debilitating Diseases
Renopathology Tipping Point: Deciphering the Molecular Code of Stage 2 Chronic Kidney Disease
The molecular events of Stage 2 CKD, from inflammation to lipid metabolism, offer insights for diagnosis and treatment.
Chronic & Debilitating Diseases
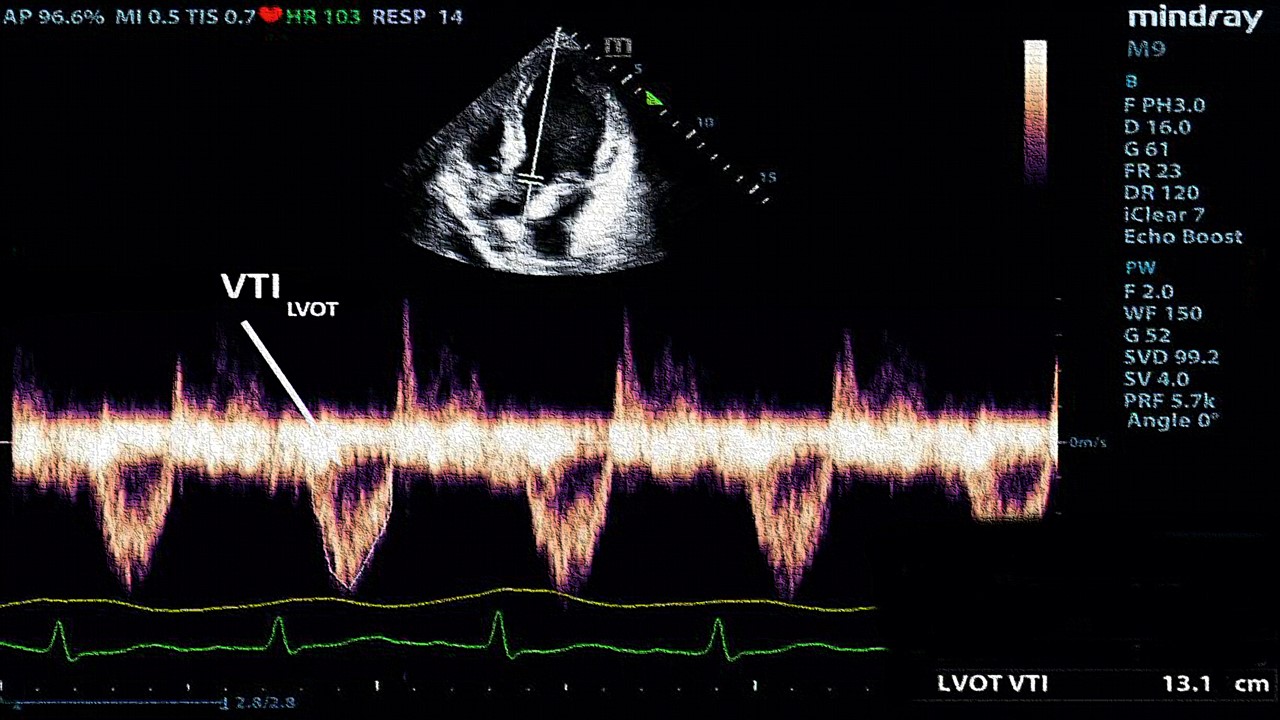
A New Lens on Shock: Hemodynamic Insights Through Critical Care Ultrasound
CCU has transformed the hemodynamic assessment of shock, delivering a reliable, reproducible, and non-invasive tool for ICU clinicians.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.