Immuno-oncology has made commendable strides in recent times, showing the potential therapeutic and curative properties of recruiting the immune system in the fight against cancers. Revolutionary treatments, including CAR-T and Immune Checkpoint Inhibitors, have become available, particularly for haematological malignancies – so-called “liquid” tumors. Though immune treatments have also shown success in treating some solid tumors, significant challenges remain ahead as the field matures into a position of prominence in our anti-tumor arsenal. It is critical to appreciate the fundamental differences between haematological malignancies and solid tumors to understand these challenges.
The Differences Between “Solid” and “Liquid” Tumors
“Liquid” tumors refer to cancers which affect the blood, bone marrow or the lymphatic system – such as leukemia and lymphoma. Their chief characteristic is the free circulation of tumor cells in the blood, which is why they are called haematological malignancies. This is also the main source of their differences from solid tumors, and it is also one of the reasons immunotherapies simply work better in blood cancers. Therapies such as adoptive cell transfers which rely on the expansion of engineered T-cells introduced to a patient fare better when the site of action is the blood – the home turf of the immune system. On the other hand, solid tumors present notoriously immunosuppressive environments.
Conjointly, immune-based therapies are centered around the need to recognize tumor cells through antigens – and this has been much simpler to do in haematological malignancies, which tend to express antigens of interest more uniformly, such as the CD-19 receptor which is expressed in nearly all B cells. Naturally, this also translates to a lower degree of specificity for cancer cells – as healthy B cells also express them; limiting toxicity in such cases is important. But this pales in comparison with the difficulties presented by solid tumors, which can present very heterogeneous collections of antigens – which makes targeting the entire tumor quite the task.
And, finally, there is the elephant in the room. The delivery of drugs to haematological cancers occurs systemically – through the circulatory system, which is also their intended site of action. But solid tumors are not as easily accessible; systemic delivery is an option, but this has to rely on the body to deliver the drug to the tumor. Alternatively, there is the possibility of local administration, but the story does not end there. Even after the therapeutic agents reach the site of the tumor, accessing the entirety of it is not as straightforward as it is with blood cancers.
Current Developments
Our understanding of the relationship between the immune system and tumors has grown exponentially since the advent of the first immunotherapies. We have moved past the view of immune surveillance to a more holistic approach, termed Immune Editing as described by Robert Schneider and colleagues. The concept of immune editing is critical to understanding how the relationship between immunity and the tumor evolves and changes as the latter grows. This works in three phases:
- Elimination: This is the first stage, during which the immune system still works against tumor cells to keep them in check
- Equilibrium: The second stage; some cancer cells are not eliminated by the immune system, but are instead kept dormant
- Escape: The final, immunosuppressive stage: some tumor cells have developed resistance to immune processes, and survive to multiply, eventually outnumbering the older, immunogenic generations
This is critical to understanding the tumor Microenvironment (TME) of solid tumors and how it drastically affects the efficacy of immune-based therapies. It is also critical to note that different parts of the immune system have opposing effects on tumors: dendritic, CD4 helper T 1, CD8+ T, M1 macrophages and NK cells all promote immune activity against the tumor. CD4 helper T 2, M2 macrophages, myeloid derived suppressor cells and regulatory T cells however all promote tumor growth.
The composition and diversity of different types of immune cells across the tumor microenvironment is termed the Immune Contexture, and forms an essential class of biomarkers that can be predictive of the efficacy of any immune-based treatments. It is important to appreciate that immune contexture can also vary across tissues – with cancers metastasizing to the liver often showing higher levels of immunosuppressive immune cells, which increases the effort required to activate local T-cells to fight against cancer.
CD8+ T cells are of particular importance, as they secrete cytokines for the destruction of cancer cells. However, as they remain chronically exposed to the tumor, they eventually transform to memory T cells which produce inhibitory signals for the rest of the immune system – and lose their own ability to destroy tumor cells. This phenomenon is known as T-cell exhaustion, brought about by the expression of PD-1 by CD8+ T cells. Additionally, regulatory T cells and dendritic cells (mentioned above) have also been found to be involved in the expression of CTLA4, which forms a critical part of the suppressive immune pathway of regulatory T cells. Revolutionary treatments in immuno-oncology have been created by exploiting these mechanistic understandings of the tumor microenvironment and reversing the inhibition through Immune Checkpoint Inhibitors. These treatments have played an instrumental role in re-orienting our view of immunotherapy as a potent weapon against solid tumors: ipiluminab, an anti-CTLA4 agent; and nivolumab, which acts against PD1. Their effectiveness against types of melanoma, non-small cell lung cancer, squamous cancer, colorectal cancer and others, either on their own or as combination therapies, has proven immunotherapy’s value beyond blood cancers.
Tumor Mutational Burden (TMB) is another success story for solid tumor immunotherapies. A high rate of mutations has been associated with better outcomes across multiple kinds of immunotherapies. The challenge in harnessing the potential of TMB as a biomarker was not through lack of mechanistic understanding regarding how it works, but through a lack of universal agreement on defining it. Work on harmonizing the way it is estimated has been exemplary of international efforts in oncology – or any field of science in general – and further work on its standardisation continued this year through the Friends of Cancer Research TMB Harmonization Project.
Future Developments
We stand to further harness the potential of mutational burden by artificially increasing the mutations of a tumor, through combination therapies such as radiotherapy: this can lead to the development of neoantigens which are unique to cancer cells, increasing the ability of a therapy to be specific to a cancer. Further work in genetic profiling will be required to create more robust biomarkers for immunotherapies. In a study investigating the potential for immunogenic chemotherapies to induce tumor responsiveness to immunotherapies, mutations in KRAS and EGFR showed little difference on CD8+ T cell infiltration of the tumor. However, tumors presenting TRP53 or TRP53/KRAS mutations exhibited significantly lower rates of CD8+ T cell infiltration; immunogenic chemotherapy was shown to reverse this and make immunotherapy more effective.
Another phenomenon which presents a challenge in solid tumor immunotherapies is pseudoprogression. This occurs when the tumor is enlarged subsequent to the therapy – although this is not always indicative of actual tumor growth, but rather it may indicate swelling and inflammation following a genuine immune response. This has been reported in up to ~14% of responses, and is then followed by the expected clinical benefit. Distinguishing between progression and pseudoprogression remains a key concern regarding the viability of immunotherapies, as failure to recognize true progression has obvious consequences. New frameworks, such as irRC, iRECIST and imRECIST established to differentiate between the two look promising, and indicate the need for further quorum from the industry to standardise the classification for pseudoprogression.
It is also critical to appreciate the physical challenges presented by the tumor environment to immunotherapies. For example, the T-cells may be excluded from reaching the tumor due to the expression of TGF-b, which contributed to the build-up of a collagen stroma that prevented infiltration by activated immune cells. Combination therapies with anti-PD1 and TGF-b blocking antibodies subsequently increased treatment responsiveness. Assessing such mechanisms of primary tumor immune escape, or secondary immune escape (which is demonstrated after the commencement of immunotherapy), will be key to the future of the field.
While work remains promising and innovative, and has certainly spread to a whole array of other methods we have not had the opportunity to discuss here – such as cytokines, antibody-drug conjugates and adoptive cell therapies, we illustrate why the success of immune-based therapies in solid tumors presents an entirely different field from the progress we have seen from them in haematological malignancies. Colossal efforts in improving biomarker standards, and collection of the data to drive those standards, will be critical in assessing future viability of investigational products as well as to form comprehensive understanding of the mechanistic functions that drive those products. Equally critical will be to replicate the collective efforts made with standardising TMB for other phenomena – such as the degree of pseudoprogression. This highlights the importance of exchanging ideas across the industry; Proventa International will be holding key Oncology Strategy Meetings with industry leaders in 2022 – follow the links below for more information.
Nick Zoukas, Former Editor, PharmaFEATURES



Subscribe
to get our
LATEST NEWS
Related Posts

Immunology & Oncology
The Silent Guardian: How GAS1 Shapes the Landscape of Metastatic Melanoma
GAS1’s discovery represents a beacon of hope in the fight against metastatic disease.
Immunology & Oncology
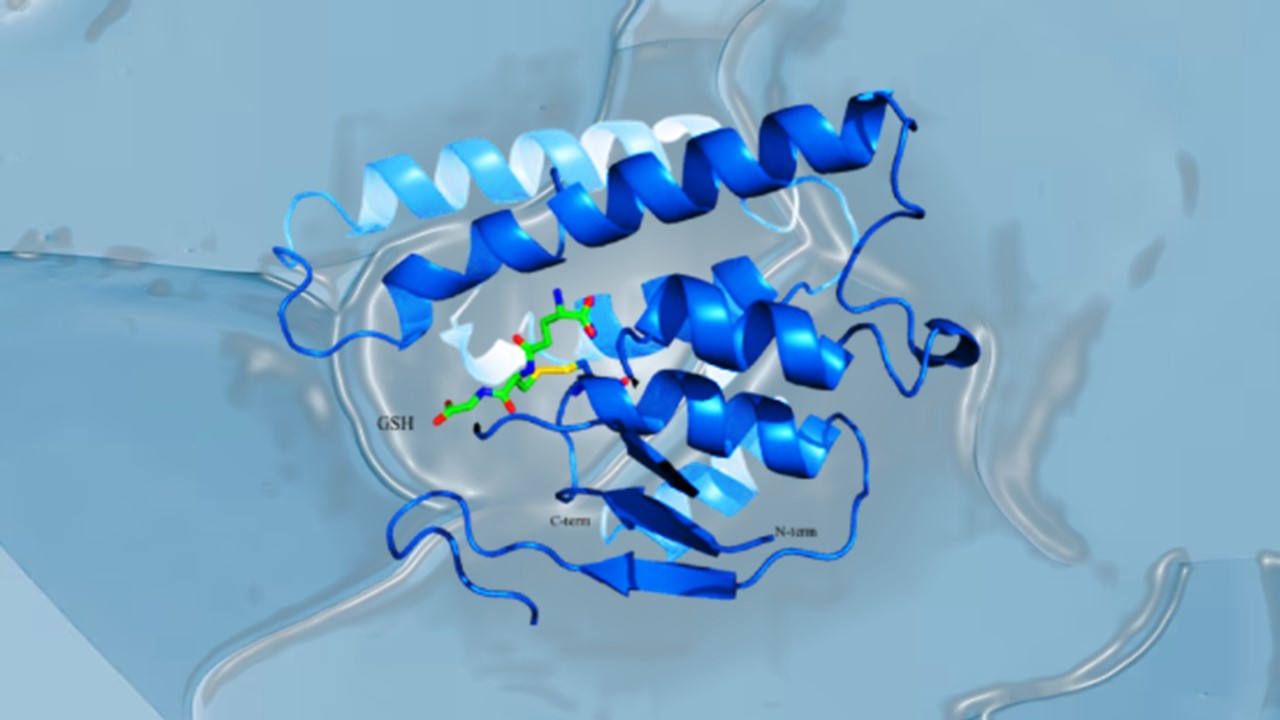
Resistance Mechanisms Unveiled: The Role of Glutathione S-Transferase in Cancer Therapy Failures
Understanding this dual role of GSTs as both protectors and accomplices to malignancies is central to tackling drug resistance.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.
Designing Better Sugar Stoppers: Engineering Selective α-Glucosidase Inhibitors via Fragment-Based Dynamic Chemistry
One of the most pressing challenges in anti-diabetic therapy is reducing the unpleasant and often debilitating gastrointestinal side effects that accompany α-amylase inhibition.