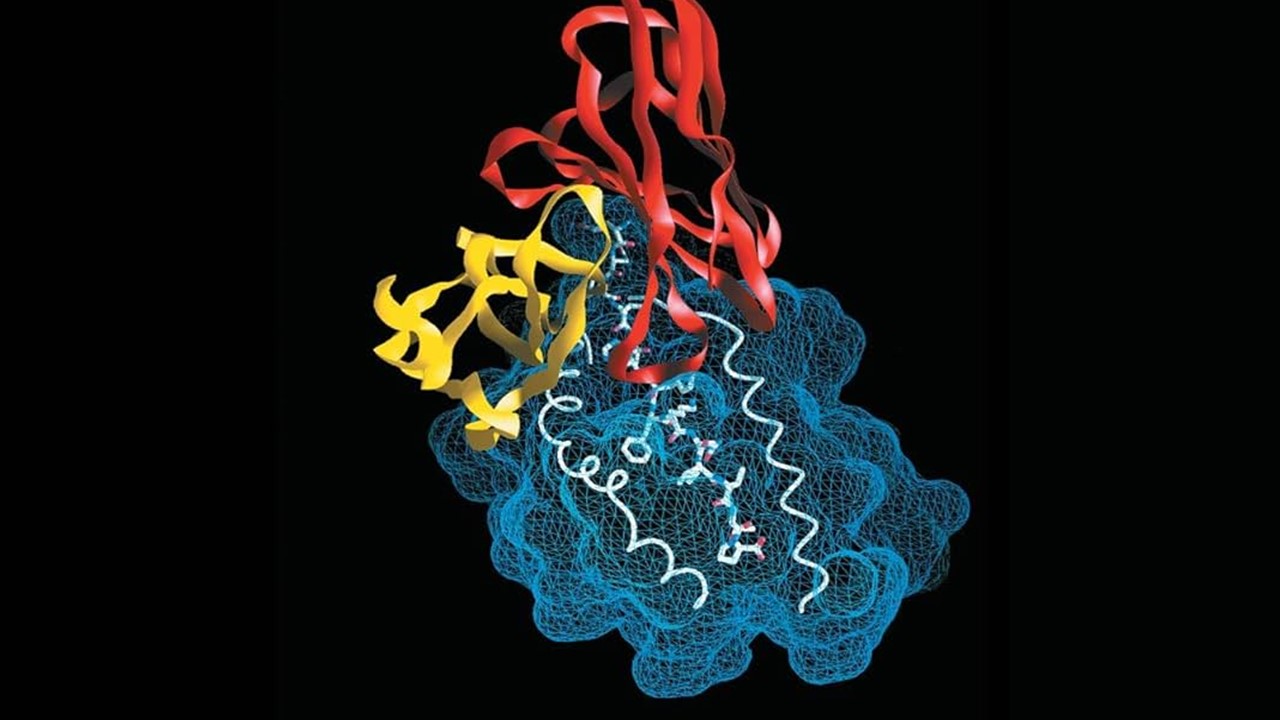
In recent decades, the landscape of drug discovery has dramatically evolved from traditional methods to more sophisticated approaches. One of the most notable advancements lies in the development of targeted liposomal therapeutics, which are reshaping our understanding of how drugs can be delivered efficiently and selectively to diseased tissues. Liposomes, lipid-based spherical vesicles, serve as carriers that encapsulate therapeutic agents, allowing them to be transported to target cells with high precision. Their transition from conventional chemotherapeutic agents to more refined, targeted drug delivery systems represents an important leap forward.
This shift from traditional drug discovery, which largely relied on broad-spectrum agents, to modern lead discovery emphasizes the increasing focus on minimizing off-target effects and enhancing drug specificity. Targeted liposomal formulations are at the forefront of this evolution, offering a means of delivering drugs directly to tumor sites while sparing healthy tissues from unnecessary exposure.
Transferrin: A Gateway to Precision Targeting
One of the most promising developments in liposomal therapeutics is the use of targeting ligands, which guide liposomes to specific cell types. Among these, transferrin (Tf) has gained significant attention. Tf receptors (TfR) are known to be over-expressed on the surface of many tumor cells, making them an attractive target for drug delivery. Tf-conjugated liposomes exploit receptor-mediated endocytosis, a process that allows the liposome to enter and release its contents within tumor cells.
The utility of transferrin-bound polyethylene glycol (PEG)-coated liposomes, also known as “stealth” liposomes, has been demonstrated as a powerful method for intracellular targeting. Tf-stealth liposomes can evade the immune system and remain in circulation for longer periods, increasing their chances of reaching tumor cells. Tf-liposomes, in particular, have been shown to accumulate in tissues like the liver and brain, indicating their potential to cross physiological barriers and access hard-to-reach tumor sites.
The Importance of Size in Liposomal Design
An often overlooked but critical factor in the effectiveness of Tf-liposomes is their size. Studies, such as those conducted by Hatakeyama et al., have demonstrated that liposomes smaller than 80 nanometers are more efficient at targeting tissues via receptor-mediated endocytosis. This size constraint is especially important for targeting tissues like the liver and brain, where small particles are more likely to penetrate and accumulate.
Interestingly, even though the heart is capable of uptaking both small and relatively large liposomes through Tf-dependent mechanisms, size regulation plays a pivotal role in conferring tissue selectivity. These findings underscore the importance of fine-tuning liposome size to optimize tissue targeting and maximize therapeutic efficacy. By adjusting the size of Tf-stealth liposomes, researchers can tailor drug delivery to specific organs or tissues, further enhancing the precision of treatment.
Folate-Modified Liposomes: Another Promising Approach
While Tf-liposomes offer a potent avenue for targeted drug delivery, they are not the only approach being explored. Folate-modified liposomes have also garnered considerable attention due to the frequent over-expression of folate receptors (FR) on tumor cells. These receptors act as gateways, allowing folate-conjugated liposomes to bind and deliver their therapeutic payload directly into cancerous tissues.
Folate-targeted liposomes have demonstrated enhanced uptake by tumor cells, resulting in improved antitumor efficacy of encapsulated drugs. In preclinical studies, these liposomes were shown to significantly increase the therapeutic effects of doxorubicin, a commonly used chemotherapeutic agent, when tested in mice with murine lung carcinoma. This enhanced efficacy was observed regardless of circulation time after intravenous injection, highlighting the robustness of folate-modified liposomes as a drug delivery system.
The Role of Antibodies in Liposomal Targeting
Another innovative strategy in the realm of liposomal therapeutics involves the use of monoclonal antibodies (mAbs) as targeting ligands. These antibodies can be designed to bind specific tumor markers, ensuring that the liposomes deliver their therapeutic cargo to the right location. One example of this is the use of anti-HER2 monoclonal antibody fragments, which have been conjugated to liposomes carrying doxorubicin. HER2 is over-expressed in certain types of breast cancer, making it an ideal target for antibody-directed liposomal delivery.
Preclinical studies have shown that liposomes equipped with anti-HER2 antibody fragments exhibit enhanced antitumor effects compared to non-targeted liposomes. This improvement in efficacy demonstrates the potential of antibody-based targeting strategies to deliver potent drugs directly to cancer cells, further reducing the risk of off-target toxicity.
PEGylated Liposomes: A Versatile Platform for Targeting
Polyethylene glycol (PEG) modification, or PEGylation, has become a fundamental technique in the development of long-circulating liposomes. By attaching PEG molecules to the surface of liposomes, researchers can extend their circulation time, enabling more liposomes to reach the target tissue. PEGylated liposomes serve as a versatile platform for various targeting strategies, including the use of transferrin, folate, and monoclonal antibodies.
Several examples of PEGylated liposomes have demonstrated enhanced therapeutic outcomes in preclinical studies. For instance, nucleosome-specific monoclonal antibody 2C5, conjugated to doxorubicin-loaded liposomes, showed increased toxicity to cancer cells and greater tumor accumulation than non-targeted liposomes. Similarly, PEGylated liposomes carrying doxorubicin and modified with anti-HER2 or folate ligands have been shown to significantly improve antitumor effects.
Integrin Targeting: Enhancing Tumor Penetration
In addition to transferrin and folate, integrin-targeting ligands like RGD peptides are being explored as a means of enhancing liposomal delivery to tumors. Integrins are cell surface receptors that play a crucial role in tumor growth and metastasis. By attaching RGD peptides to liposomes, researchers aim to exploit these receptors to achieve more effective tumor targeting.
RGD-conjugated liposomes have been shown to improve the uptake and cytotoxicity of encapsulated drugs in vitro. In animal models, RGD-modified liposomes carrying paclitaxel, a widely used chemotherapy drug, resulted in increased antitumor activity, demonstrating their potential as a powerful tool for cancer therapy.
Challenges in Liposomal Delivery Research
Despite the remarkable advancements in targeted liposomal therapeutics, several challenges remain that hinder their widespread clinical application. One major concern is the heterogeneity of tumor microenvironments, which can affect the distribution and efficacy of liposomal formulations. Tumors often exhibit variations in blood supply, extracellular matrix composition, and cellular makeup, making it difficult for liposomes to penetrate and accumulate uniformly within the tumor. This variability can lead to suboptimal drug delivery and reduced therapeutic outcomes.
Additionally, the stability of liposomal formulations poses another challenge. Factors such as enzymatic degradation, physical instability, and the potential for premature drug release can compromise the efficacy of liposomal carriers. Researchers are actively exploring various strategies to enhance the stability of liposomes, including the use of advanced formulation techniques and the incorporation of stabilizing agents. Moreover, the immunogenicity of some targeting ligands can also raise concerns, as the immune system may recognize these components as foreign, leading to accelerated clearance of the liposomes and reduced effectiveness.
Addressing these challenges requires a multidisciplinary approach that combines insights from pharmacology, materials science, and molecular biology. By continuing to investigate the complexities of liposomal delivery and optimizing formulation strategies, researchers can further enhance the therapeutic potential of these innovative drug delivery systems.
Toward a Future of Precision Medicine
The evolution of targeted liposomal therapeutics from traditional drug discovery methods marks a significant shift in how we approach disease treatment. By leveraging the unique properties of targeting ligands like transferrin, folate, and monoclonal antibodies, as well as the versatility of PEGylated liposomes, researchers are paving the way for more precise, effective, and less toxic therapies. As this field continues to evolve, it holds immense promise for revolutionizing the way we treat cancer and other diseases, bringing us closer to the era of precision medicine.
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES
Subscribe
to get our
LATEST NEWS
Related Posts
Medicinal Chemistry & Pharmacology
Aerogel Pharmaceutics Reimagined: How Chitosan-Based Aerogels and Hybrid Computational Models Are Reshaping Nasal Drug Delivery Systems
Simulating with precision and formulating with insight, the future of pharmacology becomes not just predictive but programmable, one cell at a time.
Medicinal Chemistry & Pharmacology
Coprocessed for Compression: Reengineering Metformin Hydrochloride with Hydroxypropyl Cellulose via Coprecipitation for Direct Compression Enhancement
In manufacturing, minimizing granulation lines, drying tunnels, and multiple milling stages reduces equipment costs, process footprint, and energy consumption.

Medicinal Chemistry & Pharmacology
Decoding Molecular Libraries: Error-Resilient Sequencing Analysis and Multidimensional Pattern Recognition
tagFinder exemplifies the convergence of computational innovation and chemical biology, offering a robust framework to navigate the complexities of DNA-encoded science
Read More Articles
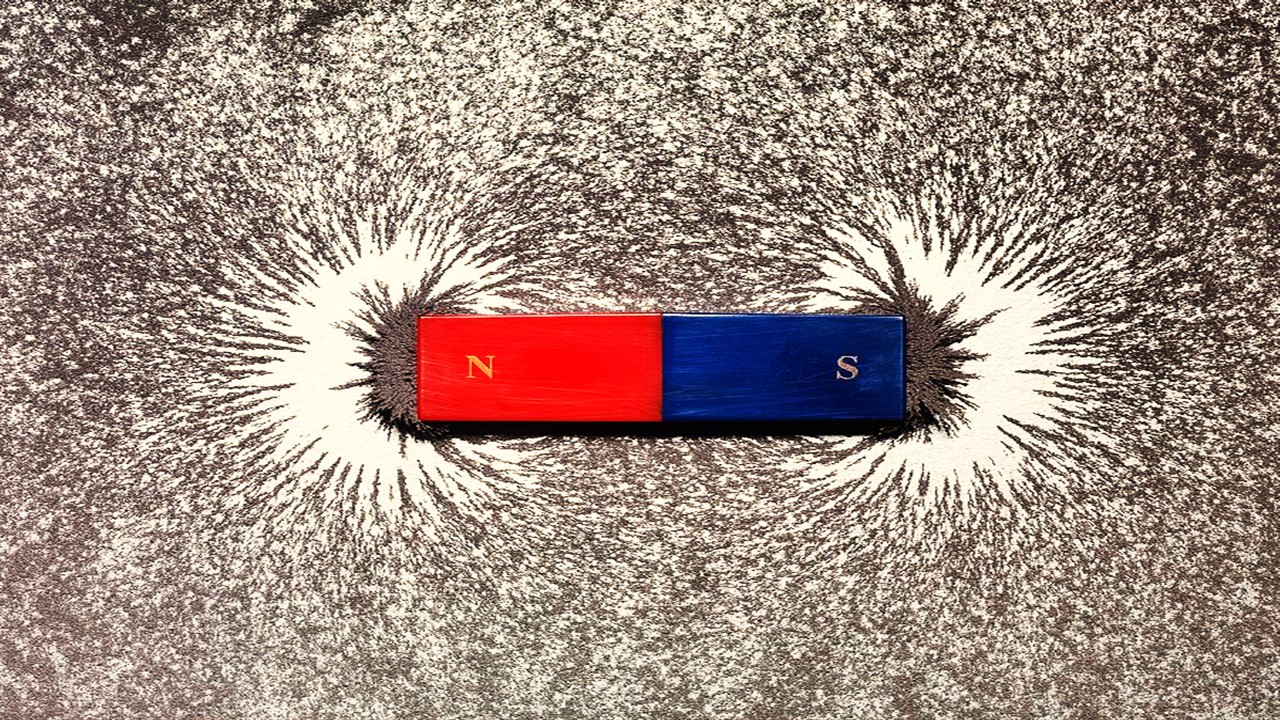
Magnetic Nanoengineering: Overcoming Biological Variability and Enhancing Therapeutic Precision
The future of nanomedicine lies in harmonizing precision, accessibility, and ecological responsibility, ushering in an era where therapies are tailored to individual biological landscapes.
Trials, Triumphs, and Trials Ahead: Navigating the Landscape of Randomized Controlled Trials in Artificial Intelligence-Driven Healthcare
The adoption of artificial intelligence in clinical practice has prompted a surge in randomized controlled trials, highlighting a balance of enthusiasm and prudence.
Illuminating the Dark Genome: Uncharted Frontiers in Therapeutic Discovery
The dark genome is not a biological void but a frontier awaiting illumination.