Despite the vast investment of research funds in nanoparticle-based drug delivery, the transition from laboratory innovation to clinical application remains disproportionately low. This is particularly evident when considering the molecular and surface chemistry of nanoparticles. Although research publications in the field exceed tens of thousands annually, only a small fraction focuses on drug delivery applications. The reason for this disparity lies in the intrinsic chemical complexities of nanoparticle surfaces, which dictate how these materials interact with biological systems.
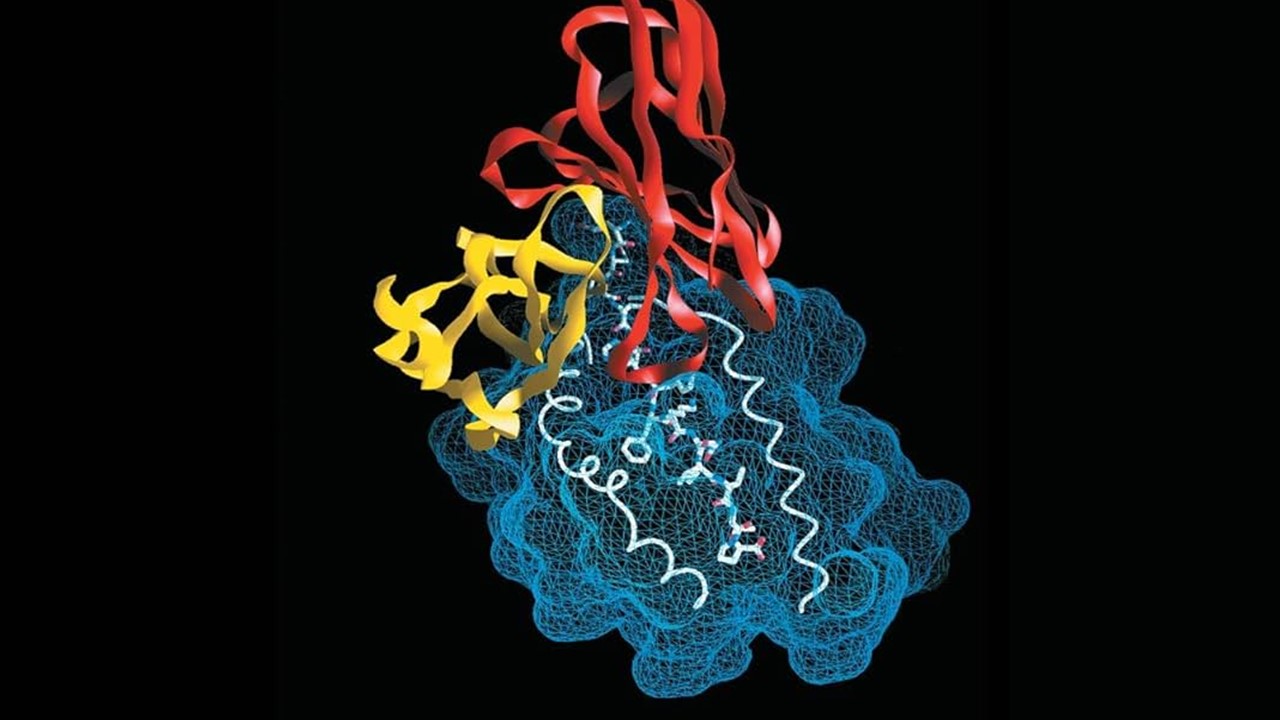
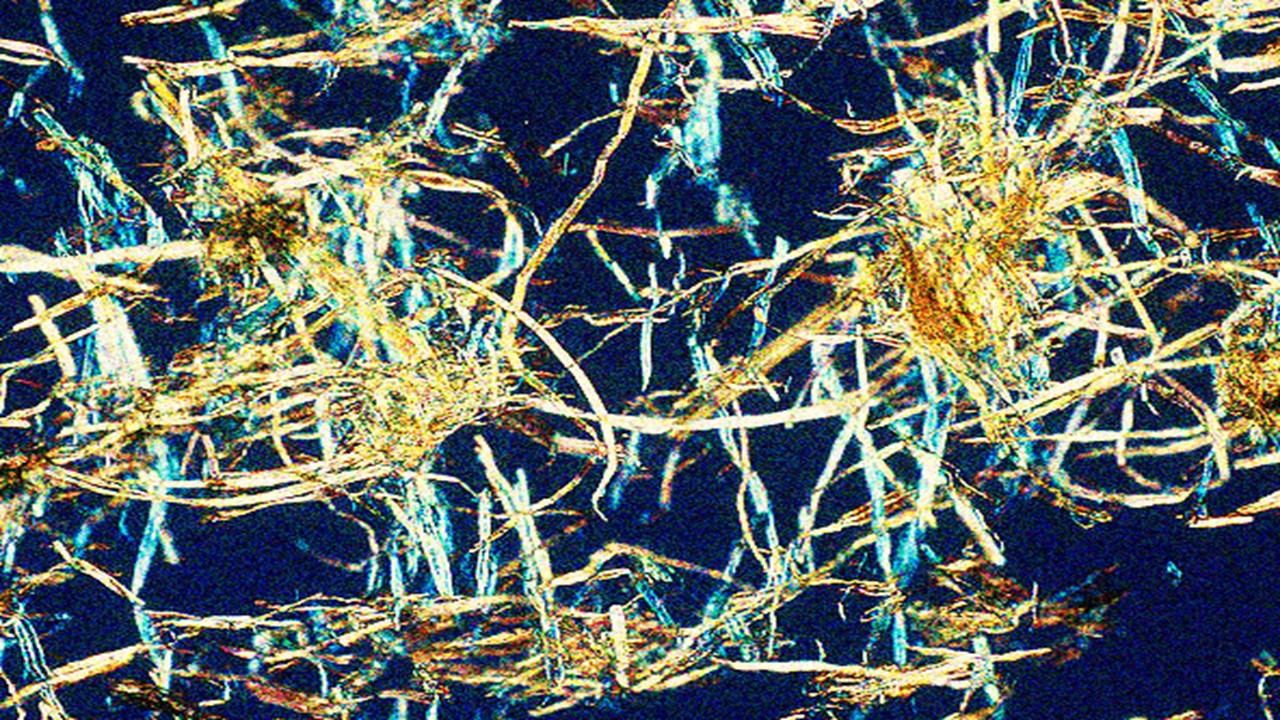
Nanoparticles, with their high surface area-to-volume ratio, exhibit unique surface chemistries that are difficult to control in physiological environments. This is especially problematic in drug delivery, where surface characteristics such as charge density, hydrophobicity, and functional group availability directly influence the particle’s pharmacokinetics and biodistribution. Surface-modified nanoparticles – such as those decorated with polyethylene glycol (PEG), lipids, or block copolymers – often show promise in laboratory settings. However, the successful translation of these chemical modifications into clinical contexts has been limited by challenges in scaling, reproducibility, and immune system interactions. These issues are compounded by the fact that nanoparticles are inherently prone to protein corona formation, a process wherein proteins adsorb onto the nanoparticle surface, altering its chemical behavior and diminishing its intended functionality.
Immune Clearance: The Achilles’ Heel of Nanoparticle Drug Delivery
A fundamental challenge in nanoparticle therapeutics is the clearance of these particles by the immune system, a process driven by the physicochemical properties of the nanoparticle surface. The reticuloendothelial system (RES), particularly through macrophage-mediated phagocytosis, identifies nanoparticles as foreign bodies primarily due to opsonization—where proteins such as immunoglobulins and complement factors bind to the nanoparticle. This protein adsorption, also known as the protein corona, is heavily influenced by the surface charge, hydrophilicity, and molecular architecture of the nanoparticle. Nanoparticles with high positive or negative zeta potentials are particularly prone to rapid immune recognition, as their charged surfaces promote strong electrostatic interactions with opsonizing proteins.
Surface modifications have been employed to reduce these interactions, with PEGylation being the most widely used technique. PEG’s hydrophilic nature creates a steric barrier, reducing protein binding and thus evading immune detection. However, the hydrophobic core of many nanoparticles remains vulnerable to RES clearance, as even minimal protein adsorption can trigger immune responses. In preclinical studies, many of these factors are overlooked, leading to overestimations of a nanoparticle’s potential efficacy in vivo. Furthermore, these immune interactions vary significantly across species, meaning that promising results in rodent models often fail to translate to human patients. This discrepancy is rooted in the molecular differences in immune proteins and cellular receptors between species, complicating the preclinical evaluation of nanoparticle formulations.
Surface Modifications: The Chemical Tactics of Extending Nanoparticle Lifetimes
To overcome rapid immune clearance, a wide range of chemical strategies has been employed to modify the surface of nanoparticles. Natural polymers such as chitosan and dextran offer advantages due to their biocompatibility and biodegradability. Chitosan, a cationic polysaccharide, interacts with negatively charged cell membranes, enhancing cellular uptake. However, its positive charge also increases opsonization, making it less suitable for long-circulating nanoparticles without further modification. Dextran, a neutral polysaccharide, fares better in circulation due to its lower immunogenicity but requires functionalization to attach to nanoparticle surfaces effectively.
Synthetic polymers, such as poly(lactic-co-glycolic acid) (PLGA) and poly(amidoamine) (PAMAM) dendrimers, offer even greater versatility. PLGA is FDA-approved for drug delivery, owing to its favorable biodegradation into lactic acid and glycolic acid, two naturally occurring metabolites. However, its hydrophobic nature promotes protein adsorption, necessitating further modifications such as PEGylation or acetylation to enhance circulation time. PAMAM dendrimers, with their highly branched architecture and amine-terminated surface groups, are ideal for multivalent interactions with drugs and targeting ligands. Nonetheless, the highly cationic surface of PAMAM dendrimers requires chemical masking (e.g., PEGylation) to reduce toxicity and prevent rapid clearance.
PEGylation: The Chemical Stealth Mechanism and Its Caveats
PEGylation, the conjugation of polyethylene glycol chains to nanoparticle surfaces, remains one of the most effective chemical modifications for enhancing circulation time. By reducing surface hydrophobicity and charge, PEGylation minimizes protein adsorption and creates a hydrophilic “stealth” layer that shields the nanoparticle from immune detection. PEG chains, typically ranging from 2,000 to 10,000 Daltons in molecular weight, increase the hydrodynamic radius of the nanoparticle, thereby reducing renal filtration and extending its half-life in the bloodstream.
However, PEGylation introduces its own set of chemical challenges. PEGylated nanoparticles are prone to aggregation under physiological conditions due to the dense packing of PEG chains, which can lead to reduced stability and altered pharmacokinetics. Additionally, PEGylation can negatively impact the nanoparticle’s ability to release its therapeutic payload. For example, PEGylated liposomes and micelles often exhibit delayed drug release kinetics, as the dense PEG layer acts as a diffusion barrier. Moreover, the molecular weight and surface density of PEG play critical roles in determining the efficacy of the modification. Higher molecular weight PEGs, such as PEG5000, extend circulation time more effectively than their lower molecular weight counterparts, but they also increase the particle’s overall size, which can limit tissue penetration and cellular uptake.
Chemical Consequences of PEG Immunogenicity
The long-term safety of PEGylated nanoparticles has recently come into question due to the rising prevalence of anti-PEG antibodies in both animal models and humans. The development of these antibodies, primarily of the IgM class, accelerates the clearance of PEGylated nanoparticles via complement activation and macrophage recognition. Chemically, once these antibodies bind to PEG, the particle is tagged for rapid immune clearance, nullifying the benefits of PEGylation. This presents a significant challenge for the development of PEGylated therapeutics, as repeated dosing with PEG-containing drugs may lead to an adaptive immune response that compromises both efficacy and safety.
Increased clearance rates of PEGylated nanoparticles have been observed in multiple studies, particularly in the presence of pre-existing anti-PEG antibodies. This phenomenon, known as the “accelerated blood clearance” (ABC) effect, highlights the need for alternative surface modifications or the development of immunotolerant PEG derivatives. Researchers are currently investigating strategies such as using zwitterionic polymers or biodegradable PEG analogs to overcome these immune challenges. However, any modifications must maintain the delicate balance between enhancing circulation time and preserving drug delivery efficacy.
Alternatives to PEGylation: Exploring New Chemical Frontiers
As the limitations of PEGylation become increasingly evident, alternative surface modification strategies are gaining traction. Acetylation, for example, offers a chemically simpler approach to modifying nanoparticle surfaces, increasing circulation time without the steric hindrance introduced by PEG. Acetylated nanoparticles have shown comparable retention times to PEGylated particles in preclinical models, but their targeting ability may be compromised due to changes in surface chemistry that affect ligand-receptor interactions.
Other strategies focus on using endogenous biomolecules such as exosomes or lipoproteins, which offer a biomimetic approach to nanoparticle design. Exosomes, naturally occurring vesicles that mediate intercellular communication, provide an immune-evasive platform for drug delivery. Chemically, exosomes possess a lipid bilayer and surface proteins that allow them to interact with cellular membranes and evade RES clearance. However, the chemical complexity of exosomes makes them difficult to manufacture at scale, limiting their widespread use. Similarly, lipoprotein-based nanoparticles leverage the body’s endogenous transport mechanisms but require precise chemical manipulation to ensure stability and targeting specificity.
Moving Forward: The Chemical Pathway to Clinical Translation
To bridge the gap between laboratory research and clinical application, future efforts must focus on optimizing the chemical properties of nanoparticles to improve their interaction with biological systems. Preclinical models must better mimic human physiology, particularly regarding immune system interactions. One potential approach is to develop humanized animal models that more accurately reflect the human immune response, allowing for more reliable predictions of nanoparticle behavior in clinical settings.
The continued exploration of surface modifications beyond PEGylation will be crucial. Zwitterionic polymers, which possess both positive and negative charges, show promise in reducing protein adsorption without eliciting an immune response. Similarly, advances in biodegradable polymers may offer a means of evading immune clearance while maintaining the desired pharmacokinetics. These next-generation modifications will need to be rigorously tested, not only for their chemical stability but also for their ability to maintain the delicate balance between circulation time, targeting specificity, and drug release kinetics.
The chemical intricacies of nanoparticle design and modification present both opportunities and challenges for the field of drug delivery. As researchers continue to refine these strategies, a deeper understanding of the chemical interactions between nanoparticles and biological systems will be key to unlocking their full potential in therapeutic applications.
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES
Subscribe
to get our
LATEST NEWS
Related Posts
Medicinal Chemistry & Pharmacology
Aerogel Pharmaceutics Reimagined: How Chitosan-Based Aerogels and Hybrid Computational Models Are Reshaping Nasal Drug Delivery Systems
Simulating with precision and formulating with insight, the future of pharmacology becomes not just predictive but programmable, one cell at a time.
Medicinal Chemistry & Pharmacology
Coprocessed for Compression: Reengineering Metformin Hydrochloride with Hydroxypropyl Cellulose via Coprecipitation for Direct Compression Enhancement
In manufacturing, minimizing granulation lines, drying tunnels, and multiple milling stages reduces equipment costs, process footprint, and energy consumption.

Medicinal Chemistry & Pharmacology
Decoding Molecular Libraries: Error-Resilient Sequencing Analysis and Multidimensional Pattern Recognition
tagFinder exemplifies the convergence of computational innovation and chemical biology, offering a robust framework to navigate the complexities of DNA-encoded science
Read More Articles
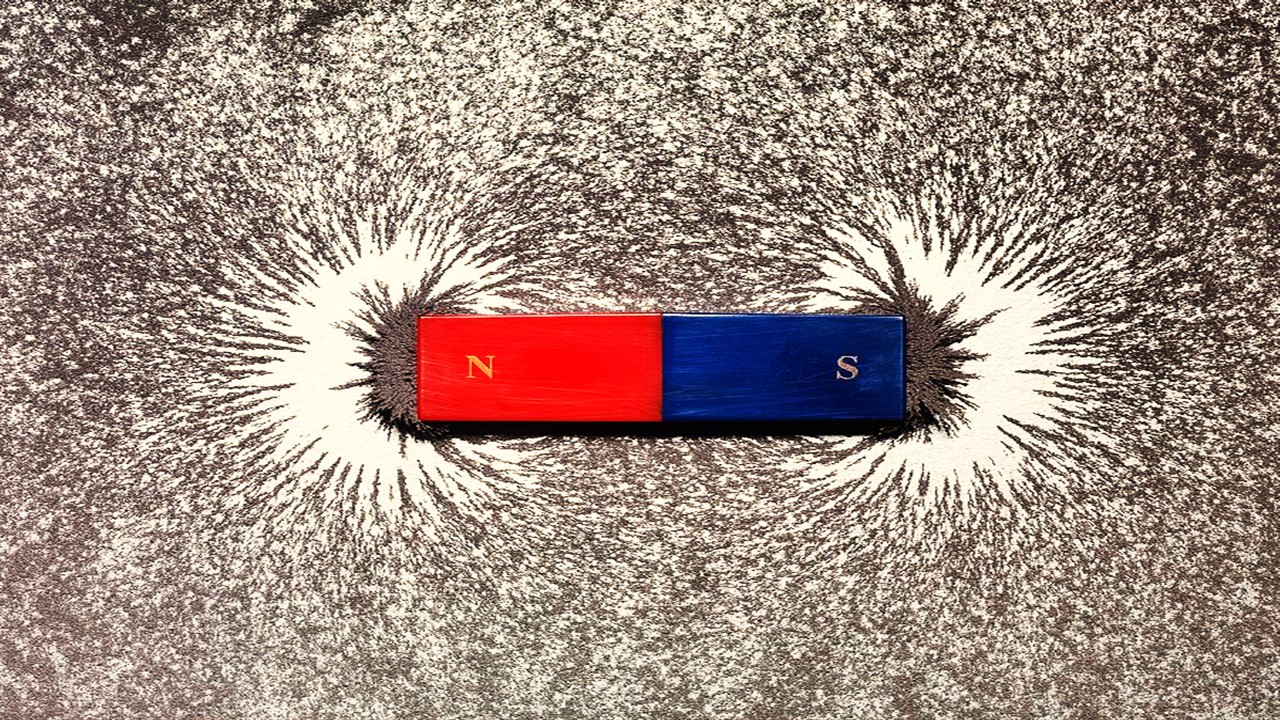
Magnetic Nanoengineering: Overcoming Biological Variability and Enhancing Therapeutic Precision
The future of nanomedicine lies in harmonizing precision, accessibility, and ecological responsibility, ushering in an era where therapies are tailored to individual biological landscapes.
Trials, Triumphs, and Trials Ahead: Navigating the Landscape of Randomized Controlled Trials in Artificial Intelligence-Driven Healthcare
The adoption of artificial intelligence in clinical practice has prompted a surge in randomized controlled trials, highlighting a balance of enthusiasm and prudence.
Illuminating the Dark Genome: Uncharted Frontiers in Therapeutic Discovery
The dark genome is not a biological void but a frontier awaiting illumination.