Patients with severe paralysis represent an unmet clinical need, with little to no therapy that can improve their condition. The emerging technology of brain computer interfaces (BCIs) offers hope for such patients, with recent advancements progressing to human clinical trials. The end goal, to provide patient groups such as the ability to regain some form of functional independence within their daily lives.
Introduction
BCI technology is an emerging area within clinical research that could have some potentially exciting applications. BCIs are computational systems that acquire brain signals, analyse them, and translate the data into commands which are relayed onto an output device to carry out a specific task.
The system comprises four sequential components: (1) signal acquisition, (2) feature extraction (3) feature translation (4) device output. The device in which Stephen Hawking communicated with for example, was not a BCI, as it was voice-activated. A voice-activated or muscle-activated communication system does not qualify as BCI, as BCIs do not utilise the normal output pathways of peripheral nerves and muscles, according to a 2021 review.
BCIs strictly measure and use the signals generated by the central nervous system (CNS). A BCI is designed to recognise and quantify brain signals that convey an individual’s intention and translate these into real time device commands that accomplish a task. In a clinical context, the goal of BCI is to “replace or restore physiological function to individuals disabled by a neuromuscular disorder”.
There are a number of ways brain signals are recorded for BCI systems including fMRI (functional magnetic resonance imaging), EEG (Electroencephalography) and MEG (Magnetoencephalography).
Emerging applications of the technology
In terms of current applications, BCIs that use scalp-recorded EEGs are the most widely researched approach. To date, the application of this non-invasive BCI system is generally limited to a low-degree of freedom in which sensorimotor rhythms have been used to control cursors, spelling devices and functional electrical stimulation of a patient’s hand.
Despite these positive indications, the precision of non-invasive EEG-based interfaces are often limited by a low spatial resolution and poor signal-to-noise ratio. Invasive methods such as intracranial EEG and intracortical microarrays however, demonstrate a number of advantages. In terms of signal acquisition. These techniques typically demonstrate better temporal and spatial resolution as the electrodes are closer to the neural tissue.
Of course, interface systems which utilise invasive methods introduce a number of challenges. The most obvious challenge is the long-term usage of invasive BCIs is limited by the complications linked to implantation surgery. In addition, the stability of recording is compromised by the displacement of electrodes which can arise in tissue.
Up until now, the most significant achievements of BCI research have been confined to the preclinical research in the lab. However, recently “Synchron received a green light from the FDA to begin a breakthrough trial of implantable brain computer interface in the US”.
The latest breakthrough
Brain data transfer company Synchron announced Jul 28, 2021 that it had received FDA approval for its flagship product, the Stentrode motor neuroprosthesis. The study will begin later this year at Mount Sinai Hospital, in which the device will be assessed for safety and efficacy in patients with severe paralysis.
The device is particularly promising as it has demonstrated a number of features which overcome the challenges of previous technologies. For example, previous approaches to BCI involved drilling into the skull and implantation of needle electrodes directly into the brain tissue. This can cause long term brain inflammation, which introduces the risk of dangerous complications.
The implantation of the Stentrode device however, is a minimally invasive procedure which takes approximately 2 hours. The device is delivered into the brain via the circulatory system, similar to the insertion of stents in the heart. In addition, the system is fully integrated within the brain with no external wires protruding from the head.
The first target for the device will be the motor cortex, in order to treat the most severe cases of paralysis. According to a recent press release “patients begin using the device at home soon after implantation and may wirelessly control external devices by thinking about moving their limbs.”.
Within the brain, specific regions will fire pre-movement without conscious acknowledgment. In other words, before you pick up a glass of water, specific neurons will fire to indicate the intention to pick up the glass a significant period of time before you think about picking up the glass. These are the signals which BCI systems such as this aim to extract and translate the input into a device which can perform the intended task.
The aim of this device is to enable patients with severe paralysis to regain some functional independence, performing tasks such as texting, emailing and accessing telemedicine. In an ongoing clinical trial for this device, known as SWITCH, data from two patients in the study demonstrated the ability to control devices and text through direct input.
Ethical considerations
Of course, a number of ethical considerations continue to be raised for computational devices that could become a permanent part of the human brain. One point raised in a recent Nature article was questioning the impact of using AI to analyse the complex data output of the brain. Specifically, the fact that AI tools introduce “an unknown and perhaps unaccountable process between a person’s thoughts and the technology that is acting on their behalf.”
Another concern surrounds data security of stored information. A point raised in the aforementioned article, was the risk of digitally stored neural data being stolen or used inappropriately by companies to whom users grant total access. The speed at which BCIs have developed recently demonstrated significant steps in complex technologies and so it is hoped that data security will evolve at the same pace in order to support these advancements.
A number of ethical questions remain to be answered in the early stages of this technology:
• How long will it take for this technology to become accessible to patients
• Who will be able to access this i.e. will certain patient populations be designated priority over others?
• How much would this technology cost, and could the cost be a dividing factor in which patients can access BCIs?
The end-goal for devices such as this, is to utilise whole-brain data transfer to support a patient population representing an unmet clinical need. The potential impact on the daily lives of patients who suffer from life-changing paralysis could be incredible, and is dependent on the success of upcoming clinical trials.
Charlotte Di Salvo, Lead Medical Writer
PharmaFeatures
Subscribe
to get our
LATEST NEWS
Related Posts
AI, Data & Technology
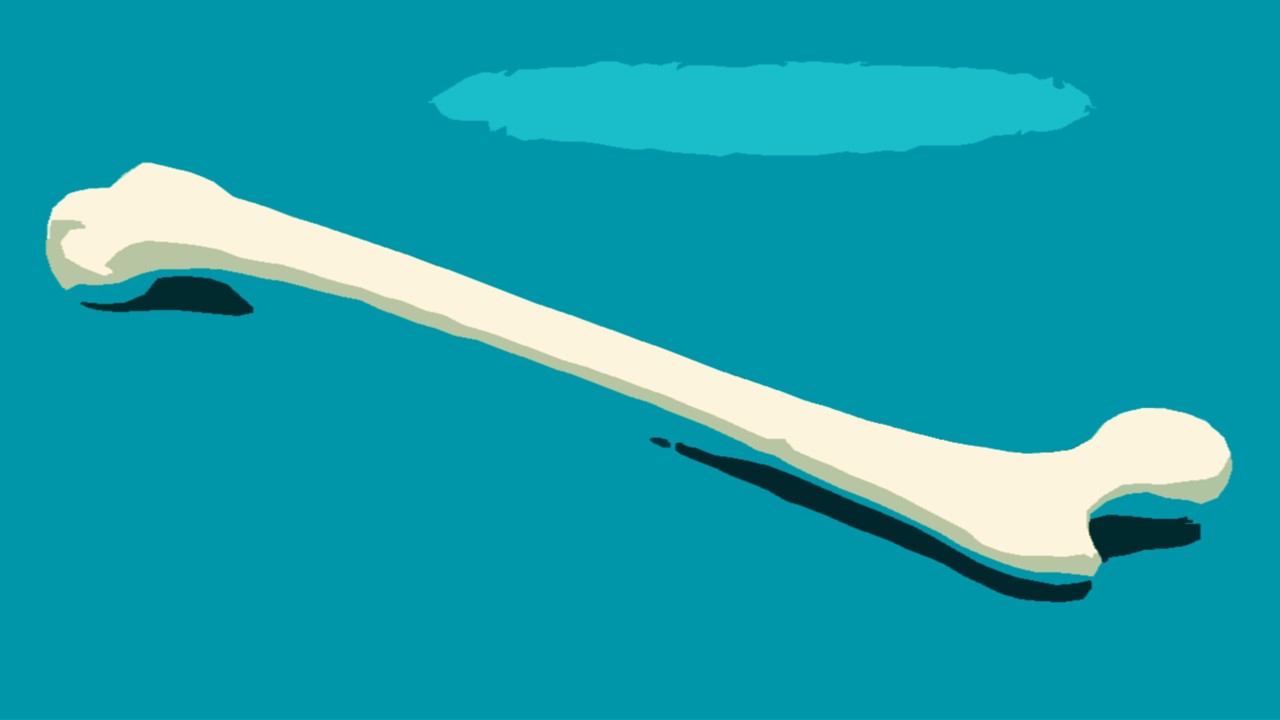
Precision in Three Dimensions: A Novel Approach to Tumor Resection and Reconstruction of the Femoral Trochanter
The integration of digital modeling and personalized guides into the surgical workflow transforms the execution of tumor resection and reconstruction.

AI, Data & Technology
Blueprint for the Future: Establishing Rigorous Standards for Medical AI Data
Medical AI requires not just vast datasets but datasets of impeccable quality.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.