As the entire world has now witnessed, the SARS-Cov-2 (COVID-19) virus does not stay still. Much like all zoonotic diseases that reach a new population, it has been rapidly evolving as it makes its way through the globe. This evolution has important implications in how society, and the pharmaceutical industry, tackle the disease.
Zoonotic Origins
With new variants emerging, it is worth remembering how the virus started. The closest related lineages of COVID-19 are all bat coronaviruses. It is reasonable to conclude that COVID-19 evolved from another bat coronavirus and then spread to humans, classifying it as a zoonosis: a disease which has only just started infecting humans by spreading from an animal reservoir. The increased likelihood of zoonotic disease as human populations encroach upon the habitats of wildlife they had never been exposed to before has been an on-going concern in the 21st century, although COVID-19 has shown that we were not adequately prepared for this eventuality.
As with all zoonotic diseases, the pathogen is rarely perfectly adapted to its new host population. The virus still maintains adaptations more suited to its ancestral hosts, which can lead to unpredictable effects on their new population. This can be seen in a variety of viruses: Ebolavirus, which is not harmful to its fruit bat hosts – but highly lethal for humans. The story is similar to the Human Immunodeficiency Virus 1 (HIV-1) which evolved from Simian Immunodeficiency Virus (SIV). Many species of SIV are non-pathogenic for their ordinary hosts – but HIV-1 is highly lethal. This trend can be justified by the fact that viruses will often evolve under the selective pressure to achieve a balance between virulence (the harm done by a virus) and infectivity (the ease with which a virus spreads).
However, COVID-19 is unlikely to be subject to pressure to become harmless; most infections occur prior to the development of symptoms – therefore high virulence does not limit transmission in this instance. Indeed, the Alpha and Delta variants, which displaced previously dominant variants in their regions, showed both a higher degree of virulence and transmission.
Emergence of Variants
The trends remain similar in COVID-19. The R0 value, the average number of other people each carrier will infect, for the dominant variants of COVID-19, in the order they appear, indicates how COVID-19 has increased in transmissibility. The lineage found in Wuhan in China, with an observed R0 of 2.4-2.6, was the earliest relative to the original virus; the subsequent dominant variants, Alpha and Beta, had an R0 +25% higher than that. The Delta variant, which has become the globally dominant variant in the latter half of 2021, has an R0 more than twice as high as non-variant COVID-19s. The R0 of the new Omicron variant has not yet been characterised outside of theoretical models, although it is estimated that it could be twice as transmissible as the Delta variant, if not more.
Evolutionary Conditions
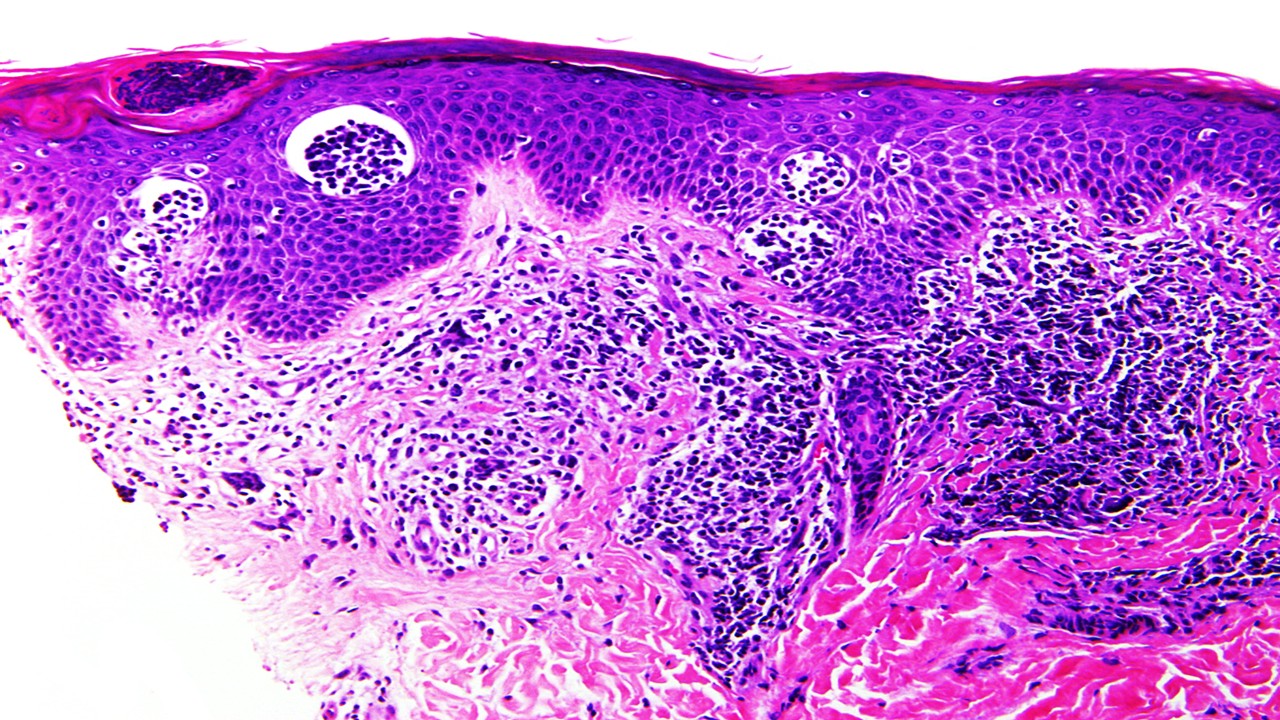
There is plenty of evolutionary space for COVID-19 to explore, given the new populations it has found itself in. However, viral evolution can be accelerated by numerous other factors as well. A factor highlighted as possibly contributing to the origin of the Omicron variant has been the high prevalence of HIV-1 in South Africa, affecting 20.4% of the country’s population. Not all of the carriers of HIV will be receiving treatment, leaving many of them to be immunosuppressed, which makes their immune systems unable to clear COVID-19 infection. Individuals that are immunocompromised from other conditions are similarly affected.
This allows the illness to become chronic in such populations, which gives it a reservoir that remains contagious and allows it to evolve. Conjointly as they receive therapeutic treatments which would ordinarily be sufficient for immunocompetent persons, the treatments act to provide further evolutionary pressure to the virus to adapt resistance to them. Vaccine efficacy has been shown to be reduced in immunocompromised individuals, as well. Antibody-based treatments are the best course of action, although it is imperative that the treatment must be at a neutralizing level; anything less may simply make it adapt. However, such therapies are prohibitively expensive for mass adoption.
That is not to say that the Omicron variant, or others, must have evolved in chronic infections within immunocompromised hosts. It is entirely possible that they simply evolved in regions with low surveillance. This is particularly important to consider when discussing the evolution of COVID-19 in the context of developing countries. This highlights the need for better infrastructure in the developing world – but is not as large an inequity of vaccine distribution. In the African continent, just 7% of the population has been vaccinated – in contrast to more than half of Europe, the UK and North America. Such low rates of immunity allow the virus to make its way through larger parts of the population, as well as enabling it to progress to severe disease that lasts longer. Both of these factors expand its margin to evolve and develop mutations.
The New Omicron Variant
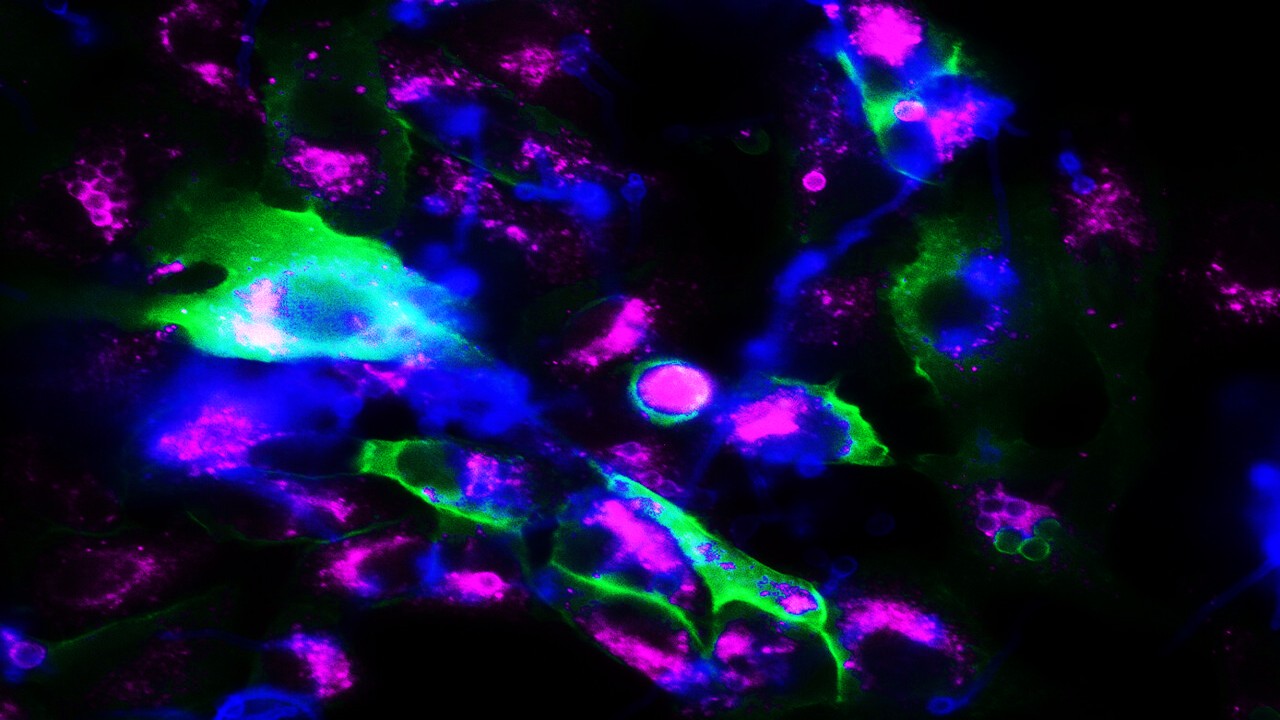
Which is why the Omicron variant, also known as the B.1.1.529 lineage, has placed the entire world on alert. The variant has over 30 mutations affecting the spike protein, which is the protein used to enter host cells and the one most often targeted by vaccines. Of these, 15 mutations are on the actual receptor-binding domain of the protein. Additionally, it also has three mutations at the furin cleavage site; one mutation at the same site was previously associated with higher infectivity in the Delta variant. Computer modelling suggests that it could evade immune responses, including from T-cells.
However, such evolutionary adaptations could come at the expense of other competencies. While it is very likely that the Omicron variant may be competent at re-infecting immunized hosts due to poor recognition by antibodies, vaccines may still confer significant benefits against severe disease. Furthermore, the adaptations that enable it to evade the immune system may reduce its replicating capabilities. It is also still possible that it preferentially binds to other parts of the respiratory system, where it is less likely to cause severe damage – such as the upper airways.
What remains certain is that life cannot move on from the pandemic while we allow the virus to evolve uncontrolled. Vaccination, and equitable access to it for the entire world, is a cornerstone of helping not only our overwhelmed health systems, but also minimizing the opportunities for evolution by the virus. Additionally, it is clear that better surveillance – with full genetic analysis of observed cases – is required throughout the world in order to detect and respond to new variants as early as possible. It is likely that in the coming weeks we will have a much better idea of what the mutation profile of the Omicron variant means with regards to its R0 value, its pathogenicity, and the implications for how we need to respond to it, both on a societal and a pharmaceutical level. But with each new variant come new uncertainties – and that is a cycle we must end.
Subscribe
to get our
LATEST NEWS
Related Posts

Infectious Diseases & Vaccinology
Enduring Blockade: Five-Year Functional Antibody Persistence Against Emerging GII.4 and GII.17 Noroviruses
Natural infection with dominant GII noroviruses elicits long-lived functional antibodies, redefining immune durability in viral gastroenteritis.
Infectious Diseases & Vaccinology
Resistant Mycosis: Reimagining Antifungal Therapy Through Mechanistic Innovation and Molecular Disruption
Emerging antifungal strategies are redefining treatment by targeting fungal physiology through diversified, mechanism-driven approaches that overcome entrenched drug resistance.
Infectious Diseases & Vaccinology
Fungal Refractory States: Deciphering Pathobiology and Therapeutic Weaknesses in the Era of Rising Antifungal Resistance
Rising antifungal resistance reflects a multidimensional biological challenge that demands mechanistically innovative, host-integrated therapeutic strategies.

Infectious Diseases & Vaccinology
Epigenetic Parasite Vulnerabilities: Repurposing Histone Deacetylase Inhibitors for Complex Multispecies Therapeutics
Repurposed HDAC inhibitors target essential parasite epigenetic machinery, offering a powerful but complex frontier for next-generation antiparasitic therapy.
Read More Articles
Spatial Collapse: Pharmacologic Degradation of PDEδ to Disrupt Oncogenic KRAS Membrane Localization
PDEδ degradation disrupts KRAS membrane localization to collapse oncogenic signaling through spatial pharmacology rather than direct enzymatic inhibition.
Neumedics’ Integrated Innovation Model: Dr. Mark Nelson on Translating Drug Discovery into API Synthesis
Dr. Mark Nelson of Neumedics outlines how integrating medicinal chemistry with scalable API synthesis from the earliest design stages defines the next evolution of pharmaceutical development.
Zentalis Pharmaceuticals’ Clinical Strategy Architecture: Dr. Stalder on Data Foresight and Oncology Execution
Dr. Joseph Stalder of Zentalis Pharmaceuticals examines how predictive data integration and disciplined program governance are redefining the future of late-stage oncology development.
Exelixis Clinical Bioanalysis Leadership, Translational DMPK Craft, and the Kirkovsky Playbook
Senior Director Dr. Leo Kirkovsky brings a rare cross-modality perspective—spanning physical organic chemistry, clinical assay leadership, and ADC bioanalysis—to show how ADME mastery becomes the decision engine that turns complex drug systems into scalable oncology development programs.
Policy Ignition: How Institutional Experiments Become Durable Global Evidence for Pharmaceutical Access
Global pharmaceutical access improves when IP, payment, and real-world evidence systems are engineered as interoperable feedback loops rather than isolated reforms.







