IL-6 is a critical mediator in the immune response, particularly in the interactions between B-cells and T-cells, which are pivotal in autoimmune diseases such as rheumatoid arthritis (RA). IL-6 promotes the differentiation of immunoglobulin-producing plasma cells, a process contributing to hypergammaglobulinemia, which is associated with chronic inflammation. This cytokine also sustains a B-cell subset known as plasmablasts, precursors to plasma cells that secrete autoantibodies. These antibodies play a role in the onset and persistence of autoimmune conditions, including RA, where chronic inflammation is a hallmark.
Understanding IL-6’s involvement in these processes has guided the development of targeted therapies like tocilizumab (TCZ), a humanized monoclonal antibody that blocks the IL-6 receptor (IL-6R). Tocilizumab is particularly effective in reducing the pathological activities mediated by IL-6, including the expansion of B-regulatory cells, reduction in pro-inflammatory cytokine expression, and enhancement of healing gene activity. Its approval for use in conditions such as juvenile idiopathic polyarthritis and giant cell arteritis underscores its wide-ranging clinical impact.
Tocilizumab’s Impact on RA Treatment and Gene Polymorphisms
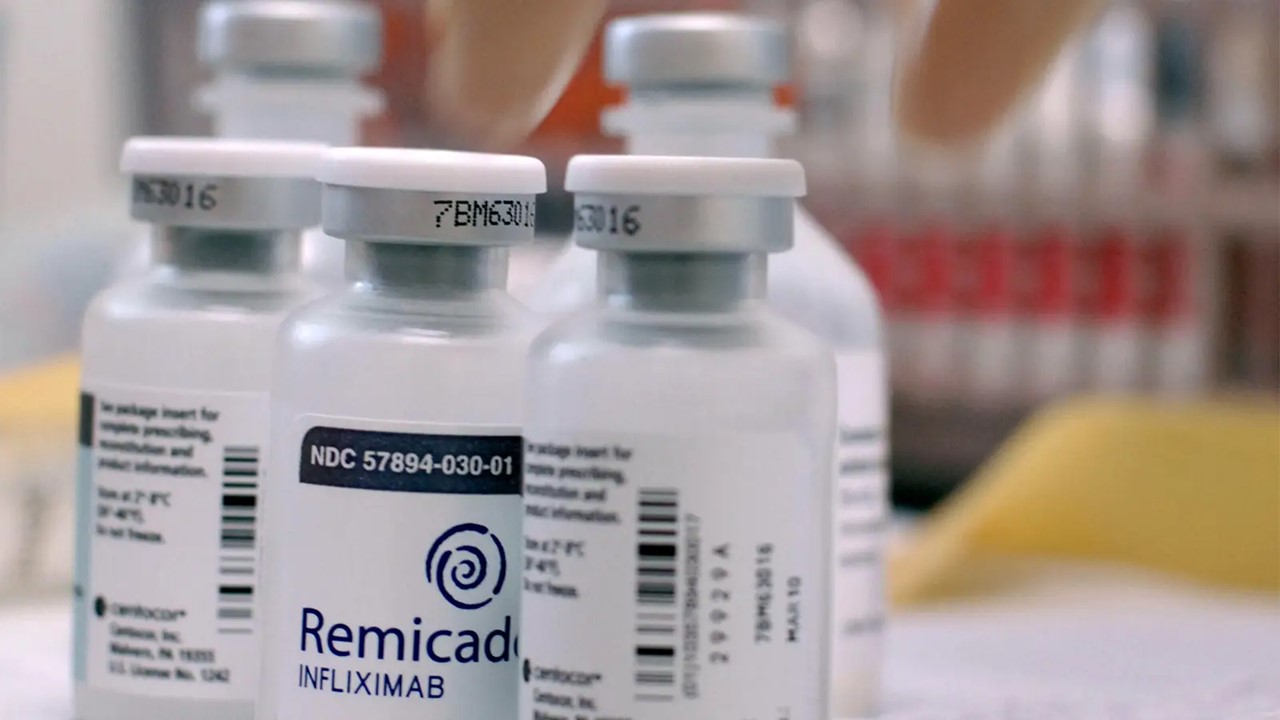
Tocilizumab offers a novel approach for patients with moderate-to-severe RA, especially those who do not respond adequately to conventional disease-modifying antirheumatic drugs (DMARDs) or tumor necrosis factor (TNF)-α inhibitors. Genetic variations in specific genes, however, can affect the therapeutic response to TCZ. For instance, studies have found that the FCGR3A rs396991-TT genotype correlates with a better response to TCZ, making it a promising predictor for treatment success in certain RA patients. This discovery enhances the potential for pharmacogenomics in tailoring therapies to individuals based on their genetic makeup.
On the other hand, while HLA-DRB1 is a well-established genetic risk factor for RA, no clear association has been identified between these alleles and response to TCZ. This underscores the complexity of RA’s genetic landscape and suggests that factors beyond the IL-6 pathway may modulate drug efficacy.
The Complexity of IL-6R Gene Polymorphisms
Further exploration of the IL-6R gene has revealed additional insights into how individual genetic differences affect therapeutic outcomes. Specifically, polymorphisms such as the AA genotype for rs12083537 and the CC genotype for rs11265618 have been shown to be strong predictors of lower disease activity (LDA) rates in patients treated with TCZ. These findings emphasize the need for more granular pharmacogenomic analysis to refine treatment approaches, allowing clinicians to optimize outcomes for patients based on their genetic profiles.
Innovations in Monoclonal Antibody Therapies
The development of newer monoclonal antibody therapies has significantly broadened the treatment landscape for RA. Drugs targeting various cytokines and pathways are being explored to enhance precision medicine for RA patients. Canakinumab, for example, targets IL-1β, a major pro-inflammatory cytokine implicated in autoimmune diseases. Although primarily used for other inflammatory conditions, its potential for RA treatment is under investigation.
Similarly, secukinumab, ixekizumab, and brodalumab, which target IL-17 and its receptor, represent a new class of therapies focused on mitigating the inflammatory processes driven by this cytokine. Research shows these drugs can be particularly effective in patients resistant to TNF inhibitors, a common challenge in RA management.
Current Diagnostic Approaches in RA
Diagnosing RA remains a complex process that involves both clinical and molecular evaluations. Traditionally, diagnostic criteria have relied on the identification of joint inflammation, presence of specific autoantibodies, and the exclusion of other potential causes of arthritis. Rheumatoid factor (RF) and anti-citrullinated protein antibodies (ACPAs) are commonly measured markers that provide strong predictive value for RA. However, recent advances in understanding the genetic and molecular underpinnings of RA have introduced more sophisticated diagnostic tools.
Emerging techniques, such as gene expression profiling and the identification of specific cytokine signatures, are helping to refine diagnostic accuracy. These methods offer a more detailed picture of the immune dysregulation in RA, allowing clinicians to better tailor treatment strategies to individual patients. Moreover, as pharmacogenomic data continue to grow, the integration of genetic information into diagnostic protocols will likely enhance early detection and improve long-term patient outcomes.
Management Best Practices: Balancing Efficacy and Safety
Effective RA management has evolved beyond the conventional “one-size-fits-all” approach, largely due to the increasing availability of biologic DMARDs. These therapies have revolutionized the treatment paradigm by targeting specific molecular pathways involved in the pathogenesis of RA. Tocilizumab, for instance, offers significant relief for patients who fail to respond to traditional DMARDs or TNF inhibitors, underscoring the importance of having multiple therapeutic options.
Combination therapy remains a cornerstone in RA management, with biologics often used alongside methotrexate or other DMARDs to enhance efficacy. However, the risk of adverse events, such as infections and cardiovascular complications, requires careful monitoring. Regular assessments of disease activity using tools like the Disease Activity Score (DAS28) and the European League Against Rheumatism (EULAR) response criteria are essential for optimizing treatment decisions. These assessments help clinicians determine whether treatment escalation or de-escalation is necessary to achieve the best outcomes while minimizing risks.
Pharmacological Advances: Precision Medicine on the Horizon
The future of RA treatment lies in precision medicine, where therapies are tailored to each patient’s unique genetic and molecular profile. Pharmacogenomic research has identified numerous single nucleotide polymorphisms (SNPs) associated with the response to biologic therapies. For instance, studies have shown that patients with specific polymorphisms in the IL-6R gene or the FCGR3A gene may respond better to certain therapies, such as tocilizumab. These insights pave the way for more personalized approaches to RA treatment, reducing the trial-and-error process currently employed.
Beyond IL-6 and TNF inhibitors, research is expanding into other cytokine pathways, including IL-1, IL-17, and IL-23. Novel agents like bimekizumab, which targets both IL-17A and IL-17F, offer promising new avenues for treatment, particularly in patients who have failed conventional therapies. Likewise, therapies targeting granulocyte-macrophage colony-stimulating factor (GM-CSF) and RANKL are showing potential in preclinical and clinical studies, suggesting that the future of RA treatment may be as diverse as the disease itself.
Charting the Path Forward
Rheumatoid arthritis remains a challenging disease with a complex etiology that combines genetic, environmental, and immunological factors. While great strides have been made in the development of biologic therapies, there is still much to learn about how to tailor treatments to individual patients. The integration of pharmacogenomics into clinical practice holds the promise of improving outcomes, reducing adverse effects, and ultimately enhancing the quality of life for RA patients.
As more is understood about the molecular mechanisms driving RA, the potential for truly personalized medicine becomes increasingly achievable. However, significant research is still needed to fully realize this potential, especially in identifying the genetic polymorphisms that influence therapeutic responses. The future of RA treatment will likely depend on this ongoing research, with the goal of providing patients with more effective, safer, and individualized therapies.
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES
Subscribe
to get our
LATEST NEWS
Related Posts

Chronic & Debilitating Diseases
Renopathology Tipping Point: Deciphering the Molecular Code of Stage 2 Chronic Kidney Disease
The molecular events of Stage 2 CKD, from inflammation to lipid metabolism, offer insights for diagnosis and treatment.
Chronic & Debilitating Diseases
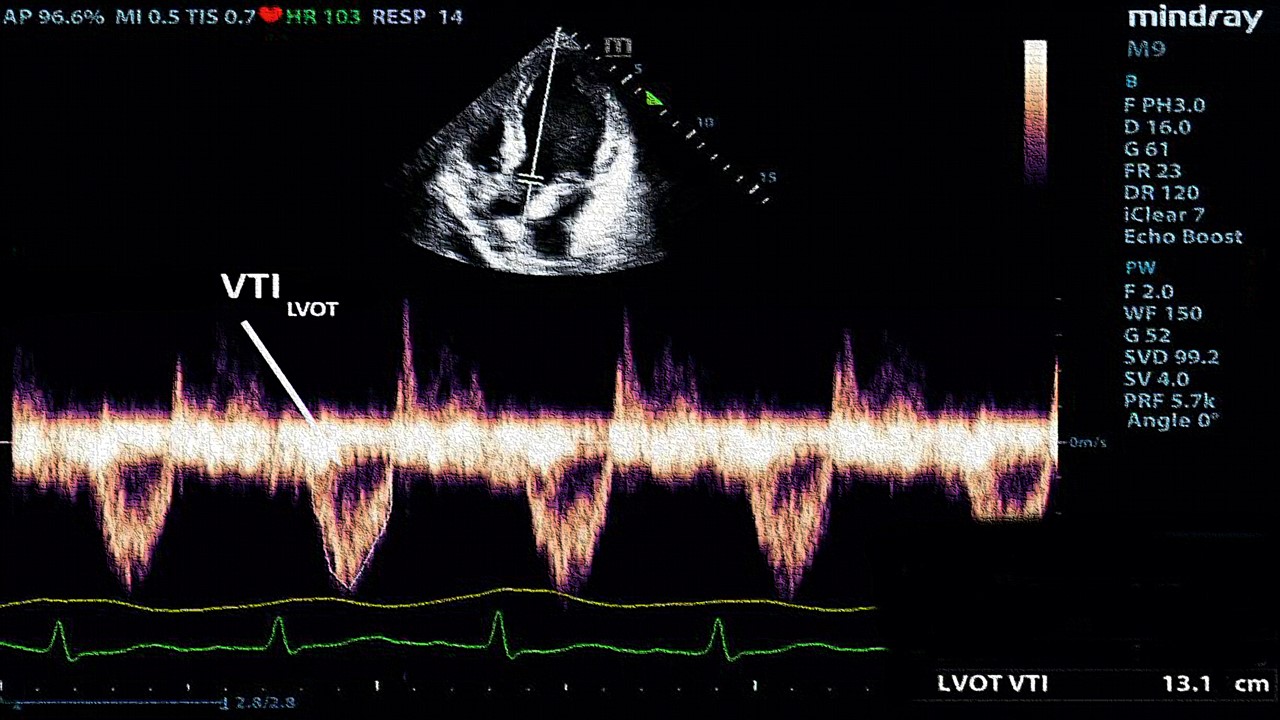
A New Lens on Shock: Hemodynamic Insights Through Critical Care Ultrasound
CCU has transformed the hemodynamic assessment of shock, delivering a reliable, reproducible, and non-invasive tool for ICU clinicians.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.