Rethinking the Blueprint of Cardiac Healing: From Cell Transplants to Molecular Reawakening
For decades, the clinical narrative of myocardial repair has rested on the hopeful shoulders of stem cell transplantation. What began as a straightforward pursuit—inject exogenous stem cells into an ischemic heart, allow them to differentiate into new muscle—has since evolved into a far more intricate and uncertain tale. Despite modest improvements in left ventricular function following transplantation of embryonic, mesenchymal, or cardiac stem cells, the formation of new cardiomyocytes within the infarct zone has remained elusive. This failure has forced the scientific community to dig deeper, shifting its gaze toward what stem cells secrete, rather than what they become.
The once-lauded cardiac stem cells (CSCs), marked by surface antigens like c-kit or Sca-1, were assumed to be the progenitors of a new generation of heart cells. However, the emerging skepticism surrounding their actual differentiation potential has led to reevaluations of their role. Clinical trials grounded in the CSC narrative have stagnated, as the reproducibility of their efficacy, and even their identity in adult mammals, came under question. The notion that resident CSCs are the workhorses of myocardial renewal began to collapse under the weight of experimental ambiguity.
Yet, rather than discarding CSCs entirely, new evidence suggests a more nuanced role—one not rooted in direct differentiation but in sophisticated, intracellular choreography. Researchers now propose that CSCs might not just float in the extracellular matrix looking for a niche to rebuild, but instead burrow into host cardiomyocytes, quietly orchestrating a regenerative ballet from within. This is not mere transplantation—it’s molecular infiltration.
The concept of intracellular CSC development introduces a second axis of myocardial regeneration, one that doesn’t require the traditional scaffold of transplanted tissue. Instead, it capitalizes on native cellular architecture, using transient amplifying cells (TACs) as intermediaries. These TACs, formed inside structures dubbed “cell-in-cell structures” or CICSs, represent a novel cellular currency in the myocardial economy. They are not stem cells, nor are they mature cardiomyocytes—they are the liminal beings that bridge both worlds.
This shift from cellular replacement to molecular reprogramming signals a paradigm shift in regenerative cardiology. No longer are we just injecting cells and hoping they integrate. Instead, we’re engineering the conditions under which the heart remembers how to repair itself—one molecule, one vesicle, one intracellular transformation at a time.
Intracellular Genesis: The Cell-in-Cell Structure as a Cardiac Engine Room
Among the most disruptive ideas to emerge in cardiac regeneration is the proposition that CSCs undergo an intracellular development process within host cardiomyocytes, forming cell-in-cell structures (CICSs). Initially identified in neonatal rat myocardial cultures and later validated across species—including adult mice, bulls, and even humans—CICSs challenge the foundational view of cardiac tissue as a static architecture of terminally differentiated cells.
Within CICSs, CSCs don’t merely lie dormant. They proliferate and undergo partial differentiation, culminating in the rupture of the host structure and the explosive release of up to 200 TACs. These TACs, small in size (10–12 μm), retain proliferative capacity and cardiomyogenic potential. They are the cellular emissaries of myocardial renewal, emerging from within the heart’s own cells rather than being delivered from external scaffolds or injectables.
Intriguingly, ischemic and hypoxic environments stimulate the formation of these CICSs. In vitro simulations of infarction showed a dramatic increase—five to tenfold—in CICS formation, suggesting that injury primes the heart not just for scarring, but also for covert regeneration. Under these stress conditions, colony formation is suppressed in favor of the intracellular route, revealing a duality in CSC fate that may be tightly governed by environmental cues.
The release of TACs from ruptured CICSs may account for the mysterious proliferation of small cardiac-positive cells observed following myocardial infarction in various models. These cells, often dismissed or mischaracterized, are now recognized as legitimate progenitors of new cardiomyocytes. Their origins within CICSs rather than traditional niches reframes how researchers interpret the regenerative response to injury.
This internal route to cardiac regeneration redefines our therapeutic targets. Instead of focusing solely on boosting CSC counts or improving engraftment, researchers can now investigate strategies to amplify CICS formation, regulate their maturation, and time the release of TACs. In this way, myocardial healing becomes a matter of orchestrating internal cell dynamics—not just injecting new materials.
The Secretome Symphony: Exosomes, MicroRNAs, and Molecular Messengers
What CSCs and their mesenchymal cousins fail to deliver through differentiation, they compensate for in secretion. Over time, stem cell-derived paracrine signaling has emerged as the primary driver behind observed improvements in cardiac function following cell therapy. These secretions, collectively known as the stem cell secretome, include cytokines, growth factors, messenger RNAs, and the ever-enigmatic microRNAs—most of which are transported in exosomes.
Exosomes, nanometer-sized vesicles enveloped in lipid bilayers, are now central players in regenerative cardiology. Their content is not random. Rather, it is a curated library of molecular instructions. In the case of cardiosphere-derived exosomes, the enrichment of miR-146a demonstrates their ability to modulate cardiomyocyte apoptosis, angiogenesis, and proliferation. When exosome production is pharmacologically inhibited, these regenerative effects diminish—a powerful testament to their functional significance.
Interestingly, exosomes do more than deliver signals—they also reflect the physiological state of their cells of origin. During acute myocardial infarction, exosomes from damaged cardiomyocytes contain a unique signature rich in survival and growth cues. Hypoxic conditions further augment this signal, increasing both the quantity and regenerative potency of these vesicles.
The downstream effects of exosomal signaling are multifaceted. Some reduce inflammation by modulating macrophage activation. Others promote endothelial proliferation, opening new capillary networks in ischemic zones. Certain miRNAs within exosomes, such as miR-590 and miR-199a, have even been implicated in directly reinitiating DNA synthesis in postnatal cardiomyocytes—a feat once thought impossible.
As a cell-free alternative to stem cell therapy, exosomes hold the promise of precision: they are easier to store, less immunogenic, and potentially engineerable. In the future, regenerative therapy may not rely on the logistics of cell harvesting and culture, but rather on tailored vesicles loaded with custom miRNA cocktails. The secretome, in essence, is the software update the heart has been waiting for.
Hypoxia and the Paradox of Regeneration: Starving Cells to Save Them
Hypoxia, long considered a harbinger of cell death, now occupies an ambivalent space in the cardioregenerative landscape. On one hand, oxygen deprivation drives infarction and necrosis. On the other, it stimulates the very processes that underpin myocardial renewal. This paradox arises because hypoxia does not simply kill—it also instructs.
In post-infarct environments, hypoxic stress catalyzes the appearance of small, dividing cardiac-positive cells. These are not just random survivors—they are regenerative agents. Systemic hypoxemia in animal models has demonstrated the ability to reduce oxidative DNA damage and rekindle proliferative activity in previously quiescent cardiomyocytes. Even more provocatively, hypoxia initiates the formation of CICSs, suggesting it directly engages CSCs to adopt regenerative phenotypes.
Still, the timing and intensity of hypoxia matter. While moderate hypoxia induces CICS formation and TAC release, excessive or prolonged deprivation, particularly during fetal development, may inhibit proliferation altogether. This threshold-dependent response highlights the delicate balancing act between inducing stress and ensuring survival. In the regenerative equation, oxygen isn’t just fuel—it’s a signal.
Mechanistically, hypoxia alters transcriptional landscapes. Key players like HIF-1α are upregulated, enhancing the expression of proangiogenic factors and anti-apoptotic proteins. These molecular shifts do not merely delay damage; they prepare the cardiac microenvironment to accept, nurture, and integrate regenerative elements—be they exosomes, TACs, or dedifferentiated cardiomyocytes.
It is perhaps in this context that the embryonic heart’s innate regenerative capacity finds its roots. In early development, the myocardium exists in a relatively hypoxic milieu. The fact that such conditions coincide with high rates of cardiomyocyte proliferation is unlikely to be a coincidence. Instead, it may be an evolutionary clue: to rebuild the heart, we must recreate the stress that shaped it.
Decoding Transitory Amplifying Cells: The Proliferative Middle Ground of Cardiac Renewal
Transitory amplifying cells (TACs) are rapidly emerging as the most promising cellular intermediates in myocardial regeneration. Unlike stem cells, which carry pluripotency but proliferate sluggishly and integrate poorly into mature myocardium, or fully differentiated cardiomyocytes, which are functionally robust but mitotically silent, TACs strike a delicate and powerful balance between both ends of the spectrum.
TACs originate from CSCs via two major pathways: direct colony formation or through intracellular development within cardiomyocytes, forming CICSs. Once matured within these structures, they are released en masse—hundreds at a time—into the surrounding myocardium. These cells retain a small size and heightened sensitivity to microenvironmental signals, particularly those of ischemic or hypoxic origin. More importantly, TACs exhibit elevated proliferative capacity and a directional bias toward cardiomyogenic differentiation.
Their phenotypic plasticity is both a challenge and a gift. Because TACs lose some of the stemness markers typical of their progenitor CSCs, they can be easily misidentified or dismissed as ordinary small cardiomyocytes. This has led to significant underestimation of their role in past studies. But when correctly identified, TACs reveal themselves as the true functional units of regeneration, capable of repopulating injured myocardium and restoring contractile function.
Efforts to stimulate TAC formation have focused on exploiting the biological context that gives rise to them. Hypoxia, inflammatory signaling, and cellular stress all prime CSCs toward TAC generation. Furthermore, studies suggest that certain growth factors and cytokine cocktails—especially those containing VEGF, IGF, and FGF—enhance the survival and proliferative behavior of TACs post-release. This suggests a viable therapeutic approach: preconditioned CSCs, or isolated CICSs with high TAC yield, could be deployed as regenerative agents in targeted infarct zones.
The uniqueness of TACs lies not just in their capacity to divide, but in their readiness to commit. These cells are not aimless progenitors. They are trained replacements, cells already on the cardiac path but not yet locked into terminal differentiation. Harnessing their potential means fast-tracking myocardial recovery while bypassing many of the oncological and immunogenic risks associated with pluripotent stem cell therapies. In the story of cardiac renewal, TACs are not merely a subplot—they are the linchpin.
Myocardial Memory: Dedifferentiation, Reprogramming, and Cellular Rebirth
Beyond the progenitor pathways lies a more radical hypothesis: that mature cardiomyocytes themselves may revert to a regenerative state under the right conditions. This concept, long viewed with skepticism due to the heart’s low mitotic index, is gaining empirical support through molecular and developmental biology. Dedifferentiation—the reversion of a specialized cell into a progenitor-like state—has been observed in zebrafish and neonatal mice, and increasingly, in stressed adult mammalian hearts.
MicroRNAs (miRNAs) such as miR-590 and miR-199a have been shown to push mature cardiomyocytes back into the cell cycle, catalyzing DNA synthesis and cytokinesis. These findings suggest that cardiomyocytes retain a latent regenerative program, one that is silenced but not erased. Other miRNAs, like miR-15, appear to suppress this process during postnatal development; inhibiting them can reopen the window of regeneration.
Parallel approaches in direct cellular reprogramming have explored the conversion of cardiac fibroblasts—abundant in the infarct scar—into cardiomyocyte-like cells. This process bypasses pluripotency entirely, using a cocktail of transcription factors (Gata4, Mef2c, Tbx5) to rewire cell fate. The result is a transformation not unlike turning soot into diamond, using molecular pressure instead of geological time.
The implications are profound. If existing cardiomyocytes or resident fibroblasts can be coerced into becoming new muscle, the heart may not need external help at all. Instead, therapeutic strategies could focus on molecular triggers—be they RNAs, small molecules, or transcriptional regulators—that awaken this regenerative potential. This would constitute a move from replacement to activation, from surgery to pharmacology.
Nonetheless, challenges abound. Dedifferentiation and transdifferentiation carry the risk of incomplete reprogramming, cellular dysregulation, or arrhythmogenesis. Without strict control, re-entering the cell cycle may provoke genomic instability or unintended phenotypes. Thus, the promise of myocardial memory must be approached with precision and humility. But if tamed, it offers one of the most elegant solutions to the problem of cardiac regeneration—using the heart’s own history to write its future.
Personalized Regeneration: Adapting Therapy to Patient-Specific Cardiobiology
Despite the breathtaking advances in stem cell science and myocardial regeneration, one fact remains stubbornly true: not all patients respond the same way. Variations in disease stage, comorbidities, medications, and even genetic background profoundly influence the efficacy of regenerative therapies. This has fueled the rise of personalized cardioregenerative medicine, an approach that aligns therapeutic strategies with individual biological profiles.
In cell-based therapies, responder versus non-responder phenomena are well-documented. Some patients exhibit robust improvement in myocardial function post-stem cell injection, while others show little to no benefit. These discrepancies can often be traced to differences in stem cell integration, paracrine responsiveness, or local tissue receptivity. The solution is not simply better cells—it is better matching.
Emerging models propose stratifying patients based on biomarkers predictive of therapeutic success. These include circulating miRNA signatures, cytokine levels, or tissue oxygenation profiles. By integrating such data into clinical decision-making, cardiologists can tailor interventions—whether they involve exosomes, CSCs, CICSs, or TACs—to the unique landscape of each heart.
Standardization is also essential. The field suffers from heterogeneity in trial design, outcome measures, and stem cell characterization. Establishing global open-access databases, harmonized protocols, and universal efficacy metrics would dramatically accelerate clinical translation and regulatory approval. What the field needs is not more breakthroughs, but better reproducibility.
Finally, technology integration will be key. Bioengineered scaffolds, AI-driven diagnostic tools, and organoid models offer unprecedented insight into patient-specific tissue responses. With these, it may soon be possible to simulate therapeutic outcomes before actual treatment—a kind of cardioregenerative preview based on individual biology.
The heart, as it turns out, cannot be healed by one-size-fits-all strategies. It demands attention to context, history, and nuance. Personalized regeneration is more than a catchphrase—it is the only path forward if we are to truly repair the most vital muscle in the human body.
Toward Clinical Translation: Engineering the Future of Cardiac Regeneration
The culmination of decades of cardiovascular research has brought us to a critical juncture—a moment where the biological principles of regeneration are finally within reach of clinical application. However, the road from bench to bedside remains strewn with challenges, many of which lie not in the science, but in the complexity of implementation. The task is no longer merely to prove that regeneration is possible, but to engineer systems that make it reliable, safe, and scalable.
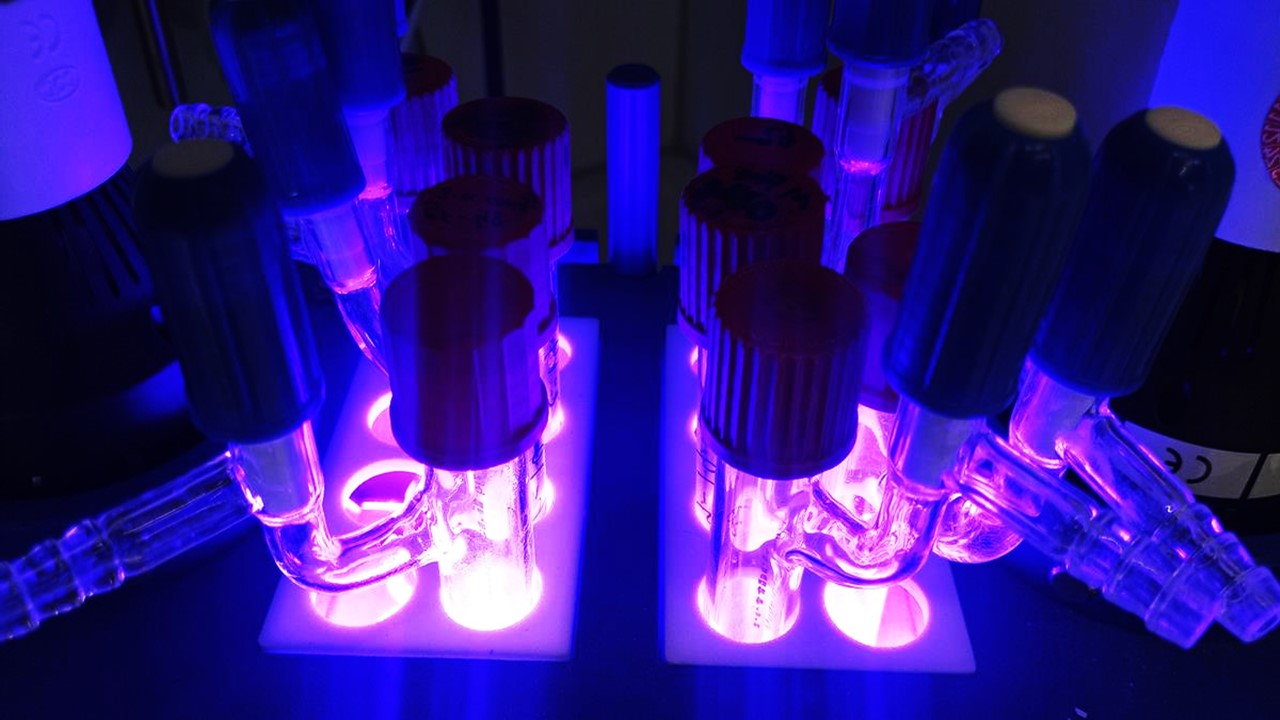
One avenue of translation is through bioengineering—specifically, the ex vivo expansion and maturation of regenerative intermediates such as CICSs and TACs. By isolating CSCs from patient myocardial biopsies, nurturing them in controlled environments, and cultivating either intracellular structures or proliferative colonies, clinicians could manufacture a ready-to-deploy regenerative product. Unlike full stem cell injections, which depend on uncertain engraftment and differentiation, these CICS-derived products would be primed for cardiomyogenic action upon delivery.
But the engineering doesn’t stop there. Delivery systems, too, must evolve. The heart is not a passive target—it contracts, perfuses, and responds dynamically to external stimuli. Microcatheters, injectable hydrogels, or smart biomaterials capable of controlled release of regenerative vesicles are now under investigation. These innovations promise targeted, temporally optimized therapy that harmonizes with the heart’s physiology.
Gene editing technologies, such as CRISPR-Cas systems, offer another translational axis. By correcting deleterious mutations or enhancing cardiomyogenic potential at the genomic level, scientists could refine the therapeutic profile of stem cells before they ever reach the patient. Such modifications could boost the expression of cardiac-specific transcription factors or suppress pathways that lead to arrhythmogenesis or fibrosis.
Moreover, integration of IT platforms into regenerative practice is rapidly transforming the field. Machine learning algorithms are being trained on vast datasets from preclinical and clinical studies to predict therapeutic efficacy, patient eligibility, and long-term outcomes. These digital companions are not just augmenting human insight—they are beginning to guide it.
Finally, regulatory and ethical frameworks must catch up with innovation. The use of intracellularly engineered structures, patient-derived cells, and vesicle-based therapies blurs the line between biologic and device, between drug and transplant. Regulatory bodies will need to develop nuanced policies that accommodate this hybridization of science. Only with regulatory clarity can industry partners invest, scale, and distribute these therapies to the patients who need them most.
In the end, the translation of regenerative science into clinical cardiology will not be accomplished by one discipline alone. It will take a symphony of molecular biologists, bioengineers, clinicians, ethicists, and data scientists. But if that harmony can be achieved, the heart will no longer be an organ sentenced to permanent scarring. It will become a system capable of renewal, a canvas for biological recovery—a testament to the triumph of intelligent design over pathological damage.
Study DOI: https://doi.org/10.1155/2020/7874109
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES
Subscribe
to get our
LATEST NEWS
Related Posts

Molecular Biology & Biotechnology
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.
Read More Articles
Designing Better Sugar Stoppers: Engineering Selective α-Glucosidase Inhibitors via Fragment-Based Dynamic Chemistry
One of the most pressing challenges in anti-diabetic therapy is reducing the unpleasant and often debilitating gastrointestinal side effects that accompany α-amylase inhibition.