Developing groundbreaking medications is an arduous journey filled with challenges and triumphs. The quest for a new drug encompasses rigorous preclinical studies in both cells and animals, followed by meticulous human clinical trials. This multi-phase process, which evaluates safety and efficacy in healthy volunteers and patients, culminates in bringing a promising drug to market. However, the reliance on animal models in this journey is not without its drawbacks, as it often leads to unforeseen failures and unsafe outcomes in clinical trials.
Drug Development Evolution and the Role of Animals
Historically, animal experiments reigned supreme in the realm of life sciences, particularly in drug development, from the 1920s to the 1970s. However, the landscape has shifted dramatically since then, with the emergence of complementary and alternative testing methods. While animal testing continues to hold sway in scientific and regulatory spheres, ethical concerns and a growing skepticism from the public have prompted a reevaluation of its efficacy and necessity.
Navigating the Challenges in Animal Testing
Animal experiments, while once considered indispensable, now face mounting challenges on multiple fronts. They are resource-intensive, time-consuming, and often fail to accurately predict human responses. This discrepancy has been underscored by the high failure rate of drug candidates in clinical trials, leading to what is known as the “reproducibility crisis” in science.
The Quest for Alternatives in Toxicology
The pursuit of alternatives to traditional animal testing, particularly in toxicology, has gained momentum in recent years. Government funding, legislative actions, and standardized guideline tests have fueled significant advancements in this arena. However, the transition away from animal models remains a complex endeavor, requiring the development and widespread acceptance of more accurate human-cell-based and computer models.
Limitations of Animal Models
Despite their longstanding role in drug development, animal models often fall short in accurately predicting human outcomes. This discrepancy has led to numerous false negatives and false positives, as well as unforeseen adverse events in human trials. Biological differences, artificial experimental conditions, and species-specific sensitivities contribute to the limitations of animal testing.
Biological Differences
One of the primary challenges in relying on animal models for drug testing lies in the inherent biological differences between animals and humans. Despite sharing many genetic and physiological similarities, there are crucial distinctions that can significantly impact the translation of results from animals to humans. These variations encompass aspects such as metabolism, organ structure and function, immune responses, and genetic makeup. For example, the way drugs are metabolized and processed in animal bodies may differ from humans, leading to discrepancies in efficacy and safety profiles. Additionally, the presence of certain receptors or signaling pathways in humans may not be accurately represented in animal models, affecting the drug’s mechanism of action and potential side effects. As a result, reliance solely on animal testing may fail to capture the nuanced complexities of human biology, limiting the predictive validity of preclinical studies.
Artificial Experimental Conditions
Another factor contributing to the limitations of animal testing is the artificiality of experimental conditions imposed on animals in laboratory settings. Animals used in research are often housed in controlled environments, subjected to standardized diets, and exposed to stressors that may not accurately mimic real-world human conditions. These artificial conditions can influence physiological responses, alter disease progression, and skew experimental outcomes. For instance, the stress experienced by animals in laboratory settings can impact immune function, hormone levels, and behavior, potentially confounding study results. Moreover, the absence of environmental factors and lifestyle variables present in human populations further complicates the extrapolation of findings from animal studies to human contexts. Thus, while animal models provide valuable insights, their utility is limited by the artificial constraints imposed during experimentation.
Species-Specific Sensitivities
The diverse sensitivities and responses exhibited by different animal species pose significant challenges in extrapolating findings to humans. Animals vary in their susceptibility to drugs, toxins, and diseases due to genetic, anatomical, and physiological differences. For example, certain drugs may elicit adverse reactions in one animal species while demonstrating safety in another, highlighting the need for species-specific considerations in drug testing. Additionally, the age, sex, and genetic background of animals can influence their responses to experimental interventions, further complicating the interpretation of study outcomes. Species-specific sensitivities also extend to differences in disease manifestation and progression, making it difficult to model human conditions accurately. Consequently, reliance on animal models alone may overlook critical aspects of human biology and pathology, jeopardizing the translational relevance of preclinical research findings.
Towards a New Paradigm in Drug Development
As we confront the shortcomings of animal models, there is a growing imperative to embrace more predictive and human-relevant alternatives. Miniature bioengineered organs-on-chips, advanced computer models, and big data mining offer promising avenues for transforming drug development. By intelligently integrating old and new methods, we can navigate the complexities of drug development more efficiently and effectively, ultimately improving patient outcomes.
Miniature Bioengineered Organs-on-Chips
Miniature bioengineered organs-on-chips represent a revolutionary approach to drug development that seeks to replicate the complex physiological environments of human organs in vitro. These microfluidic devices consist of tiny chambers lined with living human cells that mimic the structure and function of specific organs, such as the liver, heart, lung, or kidney. By recreating the intricate architecture and cellular interactions found in human tissues, organs-on-chips offer a more physiologically relevant platform for drug testing compared to traditional cell cultures or animal models. Researchers can study drug responses, toxicity, and disease mechanisms in a controlled yet dynamic environment that closely recapitulates human physiology. Organs-on-chips also enable the evaluation of inter-organ interactions and systemic effects, providing valuable insights into drug metabolism, pharmacokinetics, and toxicity profiles. Furthermore, these microscale devices offer the potential for high-throughput screening and personalized medicine applications, paving the way for more efficient and tailored drug development strategies.
Advanced Computer Models
Advanced computer models leverage computational algorithms, machine learning, and mathematical simulations to predict drug behavior, interactions, and efficacy in silico. These models integrate vast amounts of biological, chemical, and clinical data to simulate complex physiological processes and drug responses at various levels of granularity. By harnessing the power of big data and computational biology, researchers can explore drug-target interactions, pharmacokinetics, and toxicity mechanisms with unprecedented accuracy and efficiency. Computer models enable virtual screening of chemical libraries, identification of drug targets, and optimization of lead compounds, significantly accelerating the drug discovery process. Moreover, these computational approaches facilitate the design of clinical trials, prediction of patient responses, and optimization of treatment regimens, leading to more informed decision-making and improved patient outcomes. As computing power continues to advance and algorithms become increasingly sophisticated, the predictive capabilities of computer models hold immense promise for revolutionizing drug development and personalized medicine.
Big Data Mining
Big data mining involves the systematic analysis of large and diverse datasets from sources such as electronic health records, genomic databases, clinical trials, and real-world patient data. This approach enables researchers to uncover hidden patterns, correlations, and insights that can inform drug discovery, development, and clinical practice. By harnessing the wealth of information contained within big data repositories, researchers can identify novel drug targets, biomarkers, and therapeutic strategies for various diseases. Big data analytics also facilitate the identification of patient subpopulations, stratification of disease phenotypes, and prediction of treatment responses, enabling more precise and tailored interventions. Furthermore, big data mining can enhance pharmacovigilance efforts by detecting adverse drug reactions, drug interactions, and safety signals in real-time. By leveraging advanced analytics and artificial intelligence techniques, researchers can extract actionable knowledge from big data sources to drive innovation and improve patient care in the rapidly evolving landscape of healthcare and drug development.
Embracing Innovation in Drug Development
In conclusion, while animal testing has long been entrenched in drug development, its limitations are becoming increasingly apparent. As we strive to bring safe and effective medications to market, we must embrace innovation and evolution in our approach. By prioritizing human-relevant models and leveraging cutting-edge technologies, we can navigate the complexities of drug development with greater precision and efficacy, ultimately advancing the field of medicine for the betterment of society.
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES

Subscribe
to get our
LATEST NEWS
Related Posts

Drug Discovery Biology
Proteolytic Rewriting: Engineering Controlled Absence of Pathogenic Protein Persistence
Targeted protein degradation transforms drug therapy by engineering the cellular machinery to erase, rather than merely inhibit, pathogenic proteins.

Drug Discovery Biology
Open Nucleotides: Grant-Driven Infrastructure for Equitable mRNA Vaccine Manufacturing
By developing accessible cap analogs and RNA raw materials, Hongene Biotech, guided by David Butler’s expertise in nucleotide chemistry and supported by the Gates Foundation, is reshaping the molecular infrastructure that underpins global mRNA vaccine equity.
Drug Discovery Biology
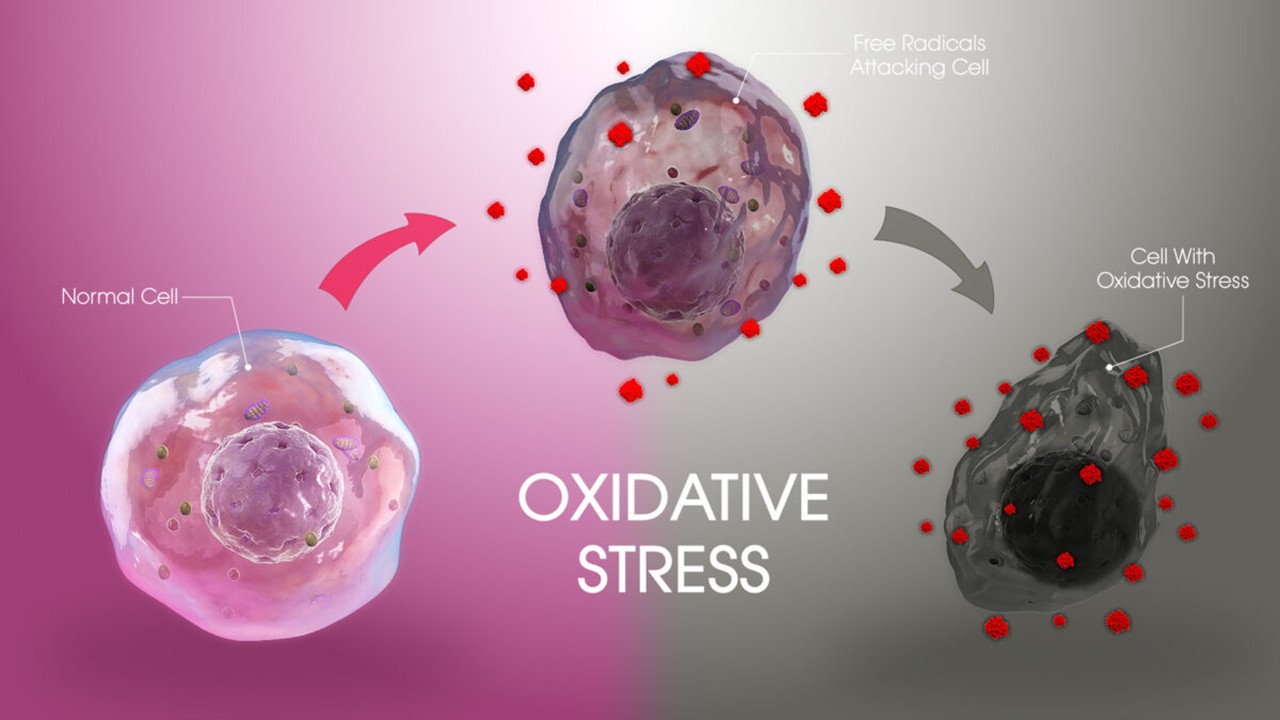
Redox Messengers: How Endogenous Gasotransmitters Rewire Vascular Biology to Resist Age-Driven Oxidative Stress
Gasotransmitters provide a biologically sophisticated means of counteracting age-related oxidative stress and preserving vascular resilience.
Drug Discovery Biology
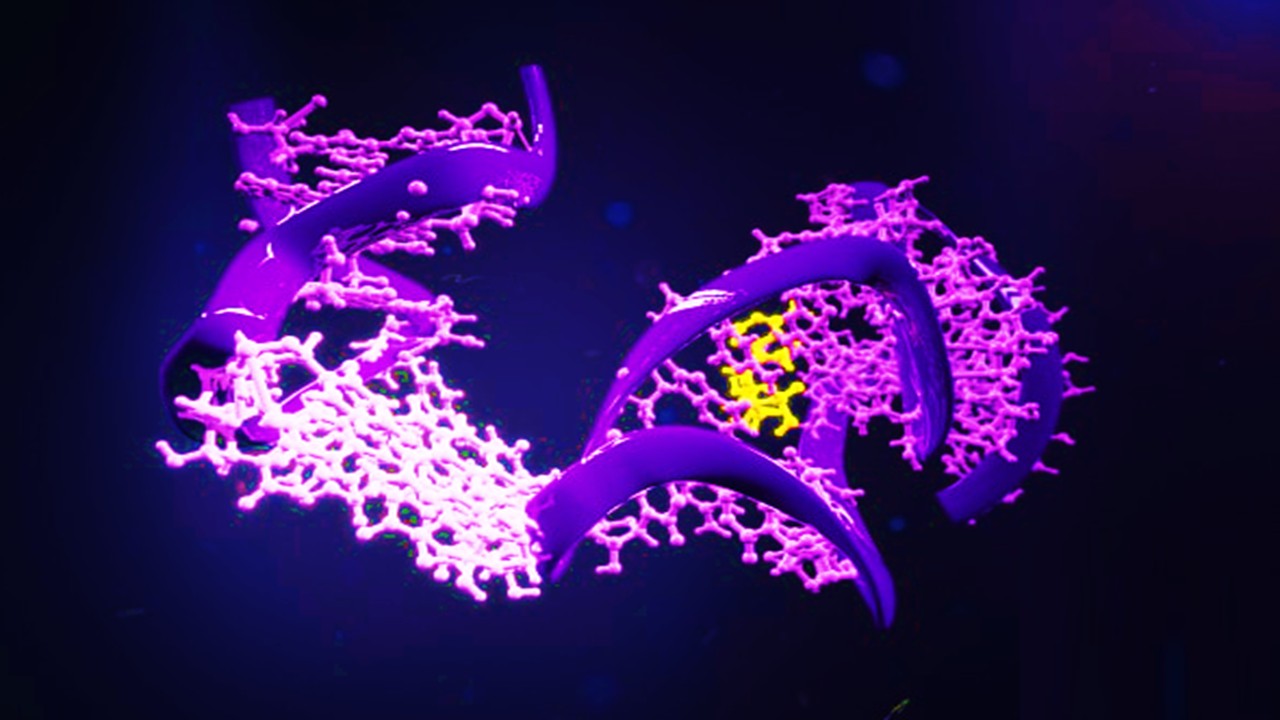
Aptamer Signal Dynamics: Engineering Nucleic Acid Recognition Systems for High-Fidelity, Multi-Modal Biosensing
Aptamers redefine biosensing by pairing programmable molecular recognition with versatile transduction strategies capable of detecting clinically relevant biomarkers with exceptional fidelity.
Read More Articles
Spatial Collapse: Pharmacologic Degradation of PDEδ to Disrupt Oncogenic KRAS Membrane Localization
PDEδ degradation disrupts KRAS membrane localization to collapse oncogenic signaling through spatial pharmacology rather than direct enzymatic inhibition.
Neumedics’ Integrated Innovation Model: Dr. Mark Nelson on Translating Drug Discovery into API Synthesis
Dr. Mark Nelson of Neumedics outlines how integrating medicinal chemistry with scalable API synthesis from the earliest design stages defines the next evolution of pharmaceutical development.
Zentalis Pharmaceuticals’ Clinical Strategy Architecture: Dr. Stalder on Data Foresight and Oncology Execution
Dr. Joseph Stalder of Zentalis Pharmaceuticals examines how predictive data integration and disciplined program governance are redefining the future of late-stage oncology development.
Exelixis Clinical Bioanalysis Leadership, Translational DMPK Craft, and the Kirkovsky Playbook
Senior Director Dr. Leo Kirkovsky brings a rare cross-modality perspective—spanning physical organic chemistry, clinical assay leadership, and ADC bioanalysis—to show how ADME mastery becomes the decision engine that turns complex drug systems into scalable oncology development programs.
Policy Ignition: How Institutional Experiments Become Durable Global Evidence for Pharmaceutical Access
Global pharmaceutical access improves when IP, payment, and real-world evidence systems are engineered as interoperable feedback loops rather than isolated reforms.
Sepsis Shadow: Machine-Learning Risk Mapping for Stroke Patients with Bloodstream Infection
Regularized models like LASSO can identify an interpretable risk signature for stroke patients with bloodstream infection, enabling targeted, physiology-aligned clinical management.







