KRAS, short for Kirsten rat sarcoma virus – named after the virus in which it was first identified, has been one of the most studied and hoped-for drug targets in oncological efforts in recent memory. This is unsurprising, given that KRAS is one of the most frequent gain-of-function mutations in epithelial cancers – and mutations on the KRAS gene are found in nearly a third of all human cancers. Yet efforts have not been as successful as the scientific community may have hoped – KRAS has presented many obstacles throughout the years, and remains one of the most elusive oncology targets.
The Hunt for KRAS
The search for therapies that can target KRAS underlies the broader trend towards more targeted therapies in oncology. Our earliest therapies, such as radiotherapy, excision and chemotherapy remain effective – but broad-acting and toxic. As our understanding of the pathophysiology of cancer has increased, so has our ability to devise targets that are unique to, or overexpressed in, tumor tissue rather than healthy tissues. Advancements in genomics, transcriptomics, epigenetics, proteomics and countless other omics approaches have been critical in providing this understanding. Yet despite being the first oncogene (tumor-promoting) to be discovered, no direct targeted therapy has been successful against it yet.
The healthy function of the KRAS gene is to produce the KRAS GTPase protein, which plays an important role in the RAS/MAPK pathway – relevant to the regulation of cellular proliferation and differentiation. The KRAS enzyme will bind to GTP and cleave it into GDP, after which it will be deactivated. “Activating” mutations that prevent this and maintain the activated, GTP-bound state of KRAS have long been associated with a plethora of different cancers – particularly colorectal, lung, pancreatic and blood cancers. This is because the activated state of KRAS will promote downstream pathways for cellular proliferation and metastasis-promoting mechanisms.
This interaction of KRAS also underlines why it is simply so hard to inhibit it through a small molecule. With no other obvious binding sites, it may seem that the only obvious option would be an agent that can occupy the GTP binding site. However, GTP has a very strong affinity for it – and is found in high cellular concentrations, making a direct small-molecule inhibitor of KRAS very challenging. However, novel drug discovery methods hold potential to change this, while targets downstream or upstream to KRAS mean that any insights gleaned regarding its pathways will retain their usefulness regardless.
Mutational Variability
It is important to appreciate that the exact mutation present on KRAS in a particular tumor will play a significant role in determining how well it could be targeted. Just one mutation is often sufficient for KRAS to be mutationally activated as a tumor-promoter. The most common mutations are G12D and G13D. Studies have gone to great lengths to establish networks of KRAS alleles and mutations across different tissues and tumor types – showing a high correlation between the genetic basis of KRAS and the effect it will have on cancer biology.
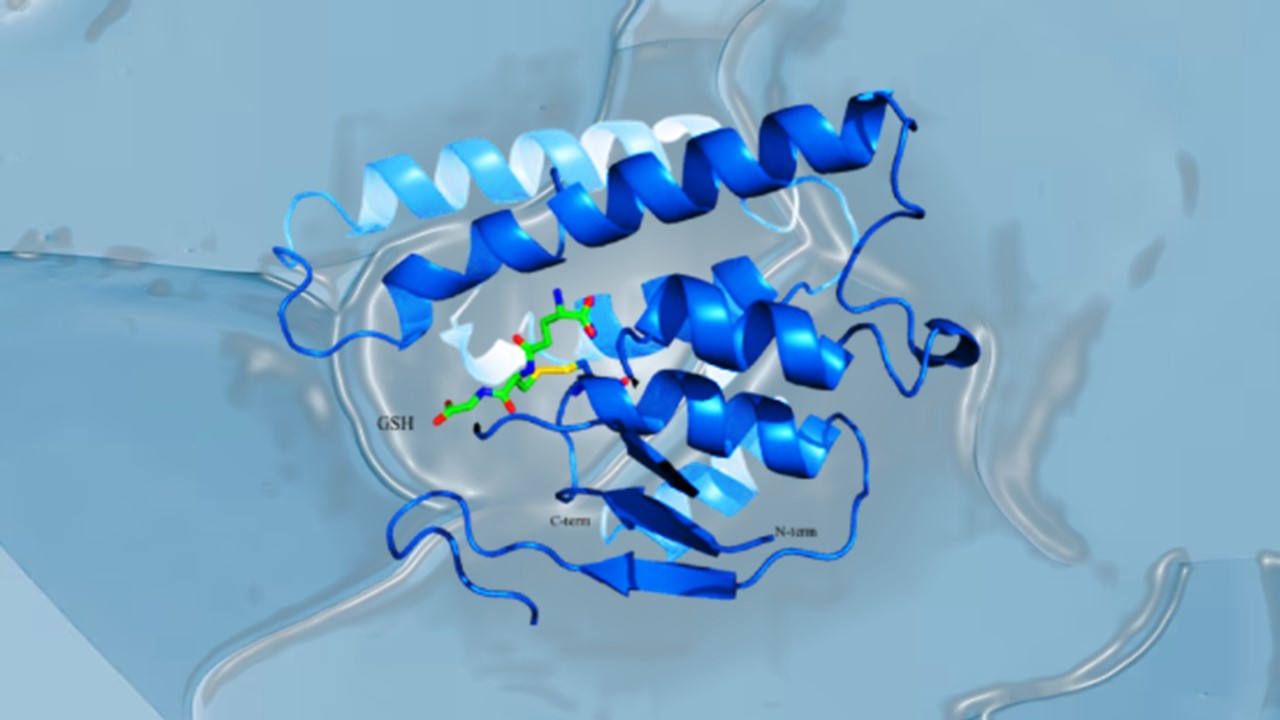
A different KRAS mutation has seen more success in being targeted through inhibitors recently, however: G12C – which may be present in up to 13% of lung cancers. Because of the way the mutated cysteine-12 affects protein folding in KRASG12C, it is located next to a cryptic pocket in the GDP-KRAS complex – known as SWII. The SWII pocket has shown potential to act as a binding site for novel targets – with agents such as sotorasib and adagrasib having shown positive results in development; the former has also received approval in the United States. The drugs work by binding on the GDP-KRAS complex and maintaining it in that inactive state, preventing them from binding to new GTP and forming active GTP-KRAS complexes.
However, both sotorasib and adagrasib will inevitably be exhausted – and the tumor they aim to treat will inevitably develop treatment resistance. Tumors have shown that they will adapt to the KRAS-G12C inhibitors – with multiple mechanisms through which to do this. One could be maintenance of the GTP-KRAS complex, which prevents the formation of the GDP-KRAS complex that the inhibitor can bind to. Alternatively, receptor tyrosine kinases may activate wild-type, non-mutated KRAS, rendering the inhibitor useless. It is important to note that immune-competent models showed a longer durable response to treatment, which bodes well for combination therapies with immune checkpoint inhibitors. Regardless, tackling the issue of resistance offers yet another hurdle to be crossed even after the herculean task of targeting KRAS is achieved.
Future Outlooks
While some forays have been made beyond targeting KRASG12C, such as with PanKRAS or RAS-targeted enzymes, those two products remain the most successful to date. Other avenues of investigation have involved the inhibition of synthetic lethal partners of KRAS – i.e. deactivation of a combination of genes downstream to KRAS, which brings about cell death. Lessons learned from this area have shown results that are highly tumor specific – e.g. IGF1R and MEK inhibition prevented growth of Non-Small Cell Lung Carcinomas (NSCLC). CDK4 inhibition also showed similar results in lung cancers, but not in pancreatic or colorectal tumors. The heterogeneity in effects suggests gaps in our own understanding of the full extent of the KRAS pathway and how genetic diversity can impact it.
Furthermore, research also implicates KRAS in the production of cytokines within the tumor microenvironment (TME), as well as a host of other immunomodulatory effects. This makes it clear that KRAS plays a role in making the TME inhospitable to the immune system. Finding ways to lessen its effects not only promises a novel target that can directly impact tumor growth, or even bring about regression, but also ways to make our own immunotherapies far more efficacious – with the immunologically exhausted TME presenting one of the largest obstacles for solid tumor immuno-oncology.
To this end, our 40-year journey since the discovery of KRAS, the first oncogene, may seem to not have yielded as much as we would have hoped for. With only two products that have been marketed – or are close to being marketed, both of which face multiple challenges, results may seem underwhelming. But our interrogation of KRAS and the pathways it underpins has yielded manifold insights that have advanced our understanding of oncology and tumor growth enormously. Continued investigation will only further expand this understanding, and perhaps lead to even more effective treatments.
Nick Zoukas, Former Editor, PharmaFEATURES
Join Proventa International’s Oncology Strategy Meeting in San Francisco to participate in closed door roundtable discussions on the role of KRAS and the potential treatments targeting it. Listen to expert-led and facilitated discussions on every topic from the cutting edge of Oncology, and meet world-renowned stakeholders and researchers.

Subscribe
to get our
LATEST NEWS
Related Posts

Immunology & Oncology
The Silent Guardian: How GAS1 Shapes the Landscape of Metastatic Melanoma
GAS1’s discovery represents a beacon of hope in the fight against metastatic disease.
Immunology & Oncology
Resistance Mechanisms Unveiled: The Role of Glutathione S-Transferase in Cancer Therapy Failures
Understanding this dual role of GSTs as both protectors and accomplices to malignancies is central to tackling drug resistance.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.
Designing Better Sugar Stoppers: Engineering Selective α-Glucosidase Inhibitors via Fragment-Based Dynamic Chemistry
One of the most pressing challenges in anti-diabetic therapy is reducing the unpleasant and often debilitating gastrointestinal side effects that accompany α-amylase inhibition.