Cardiovascular diseases (CVD) have long posed a significant threat to global health, and despite considerable advances in diagnostics and treatment, they remain a leading cause of morbidity and mortality worldwide. In recent years, nanobodies—small, stable, and highly specific antibody fragments derived from camelid heavy-chain antibodies—have emerged as a transformative tool in the field of cardiovascular diagnostics. These minuscule molecules are rewriting the playbook on how we detect, monitor, and treat cardiovascular conditions, including atherosclerosis, coronary heart disease, and von Willebrand disease.
Nanobodies, due to their unique structure, are particularly well-suited for diagnostic applications. Their small size allows them to penetrate tissues more effectively than conventional antibodies, and their remarkable stability makes them ideal for various imaging techniques. Scientists are now leveraging these properties to develop non-invasive methods for the early detection and monitoring of cardiovascular diseases, ushering in a new era of personalized medicine.
Atherosclerosis: Early Detection Using Nanobody-Driven Imaging
Atherosclerosis, a condition characterized by the buildup of plaques within arterial walls, is the underlying cause of many CVDs, including myocardial infarction and stroke. Early detection of atherosclerosis is crucial for preventing severe cardiovascular events, and researchers are now employing nanobodies to revolutionize how this disease is diagnosed and monitored.
One promising approach involves the use of nanobodies conjugated with lipid-coated decafluorobutane microbubbles, enabling contrast-enhanced ultrasound molecular imaging (CEUMI). These nanobodies target vascular cell adhesion molecule-1 (VCAM-1), a biomarker associated with early vascular inflammation in atherosclerosis. When tested in both murine models and human tissues, this imaging technique demonstrated its potential for detecting atherosclerosis in its early stages. By visualizing VCAM-1 expression, scientists could detect vascular inflammation before plaque formation reaches critical levels.
The bioconjugation process involved functionalizing the microbubbles with maleimide, allowing covalent binding with nanobodies modified to include a C-terminal cysteine thiol group. This technique, while highly promising, faced some limitations in efficiency and experimental design. Notably, the absence of normal arterial tissue in the study due to ethical constraints presented challenges in fully validating the system’s effectiveness. However, the results remain encouraging, indicating a potential pathway toward non-invasive diagnostics in clinical settings.
Beyond CEUMI, nanobody-driven positron emission tomography (PET) has also been explored as a tool for assessing atherosclerosis. Researchers utilized nanobodies targeting receptors such as the macrophage mannose receptor (MMR) and lectin-like oxidized low-density lipoprotein receptor-1 (LOX-1). PET imaging with 68Ga-labeled MMR nanobodies in rabbit models correlated with macrophage accumulation, offering a method to track disease progression at the cellular level. While this approach holds promise, challenges remain in achieving the expected in vivo results, as biodistribution in animal models does not always translate to successful human applications.
Coronary Heart Disease: Nanobodies Targeting VEGFR-2
In coronary heart disease (CHD), another prevalent and life-threatening cardiovascular condition, the ability to diagnose and monitor disease progression is critical. Vascular endothelial growth factor receptor-2 (VEGFR-2) plays a central role in angiogenesis and cell migration, making it an attractive target for diagnostic applications. Nanobodies targeting VEGFR-2 have been evaluated for their specificity and binding affinity using surface plasmon resonance (SPR) analysis. Among several candidates, nanobodies 3VGR19 and 4VR38 exhibited superior affinity, making them leading candidates for further development.
In vivo studies using radio-labeled VEGFR-2-targeting nanobodies have demonstrated rapid clearance from the bloodstream due to their small molecular size, with primary distribution in the renal system. This characteristic, while presenting challenges for therapeutic applications, is advantageous for diagnostic purposes, as it reduces background noise and allows for clearer imaging of target tissues.
Moreover, nanobodies targeting apolipoprotein B-100 (ApoB-100), a major component of low-density lipoprotein (LDL) particles, have been integrated into innovative immunosensor platforms. These nanobodies can be used to detect biomarkers associated with coronary heart disease with high sensitivity, offering a non-invasive and highly selective method for early diagnosis. By functionalizing glass carbon electrodes with streptavidin and biotinylated anti-ApoB-100 nanobodies, researchers have created sensors capable of detecting minute concentrations of ApoB-100, demonstrating their potential for clinical use in CHD screening.
Von Willebrand Disease: Nanobody-Assisted Diagnosis of Hemostatic Disorders
Von Willebrand Disease (VWD) is a hereditary bleeding disorder caused by deficiencies or dysfunctions in the von Willebrand factor (VWF), a glycoprotein critical for hemostasis, the process that stops bleeding by promoting platelet adhesion at the site of vascular injury. VWF binds to platelets and other proteins in the blood, such as clotting factor VIII, to mediate blood clot formation.
Mutations in the VWF gene lead to three major types of VWD, each varying in severity. Type 1 is characterized by a partial quantitative deficiency of VWF, Type 2 by qualitative defects that impair its function, and Type 3, the most severe form, by a near-complete absence of VWF. Acquired forms of VWD can also occur due to high shear stress conditions such as aortic stenosis or cardiomyopathies, leading to excessive cleavage of VWF.
Clinically, VWD presents with symptoms ranging from easy bruising, prolonged bleeding from minor injuries, to severe hemorrhage in extreme cases, depending on the type and severity of the disease. Diagnosing VWD requires comprehensive laboratory testing to assess both the quantity and functional activity of VWF. Assays typically include the measurement of VWF antigen levels, ristocetin cofactor activity to evaluate VWF-mediated platelet adhesion, and the factor VIII clotting activity. Specific molecular techniques may also be employed to identify mutations within the VWF gene. A promising diagnostic advancement involves nanobody-based biosensors, such as the AU/VWFa-11 nanobody, which can selectively detect the active form of VWF, allowing for the precise detection of abnormal VWF activity in patients. These innovative approaches are crucial for improving the diagnosis, classification, and management of this complex disorder.
Nanobodies are now being employed to detect VWF activity and diagnose VWD, especially in the context of cardiovascular diseases that induce high shear stress and trigger the excessive cleavage of VWF multimers.
A llama-derived nanobody, AU/VWFa-11, has been developed to specifically recognize the active A1 domain of VWF. Through SPR analysis, this nanobody exhibited excellent selectivity and has shown promise in detecting active VWF in patient plasma samples. Researchers have also applied this nanobody in immunosorbent assays to predict thrombocytopenia and bleeding risk in patients with von Willebrand disease type 2B. The assay results, which quantify the amount of VWF bound to AU/VWFa-11, have demonstrated the potential of this nanobody as a diagnostic tool, particularly in assessing the severity of VWD.
In addition to diagnosing VWD, nanobodies are being used to detect mutations in the VWF gene that contribute to various cardiovascular disorders. In a study involving 24 family members, 11 of whom carried a VWF mutation, the AU/VWFa-11 nanobody successfully identified mutated VWF monomers in plasma samples, further highlighting its diagnostic potential.
The Future of Cardiovascular Diagnostics: Personalized Medicine on the Horizon
The rise of nanobody-based diagnostic tools signals a paradigm shift in how cardiovascular diseases are diagnosed and managed. By offering unprecedented specificity and sensitivity, nanobodies enable the early detection of diseases like atherosclerosis and CHD, long before they manifest as clinical symptoms. This capability opens the door to personalized medicine, where treatments can be tailored to the individual based on real-time insights into disease progression.
The journey from traditional drug discovery to modern lead discovery has been marked by significant breakthroughs, but nanobodies represent one of the most promising advances in the field of cardiovascular diagnostics. Their small size, stability, and ability to target specific biomarkers make them invaluable in developing new diagnostic methods, particularly in imaging and biosensor technologies. While challenges remain, particularly in translating animal model results to human applications, the potential for nanobodies to transform cardiovascular diagnostics is undeniable.
As researchers continue to refine these tools and overcome existing limitations, nanobodies will likely become a cornerstone of modern cardiovascular medicine, paving the way for earlier, more accurate diagnoses and more effective, personalized treatments. The future of cardiovascular care is increasingly one where nanobodies play a central role, offering hope for millions of patients worldwide.
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES
Subscribe
to get our
LATEST NEWS
Related Posts

Chronic & Debilitating Diseases
Renopathology Tipping Point: Deciphering the Molecular Code of Stage 2 Chronic Kidney Disease
The molecular events of Stage 2 CKD, from inflammation to lipid metabolism, offer insights for diagnosis and treatment.
Chronic & Debilitating Diseases
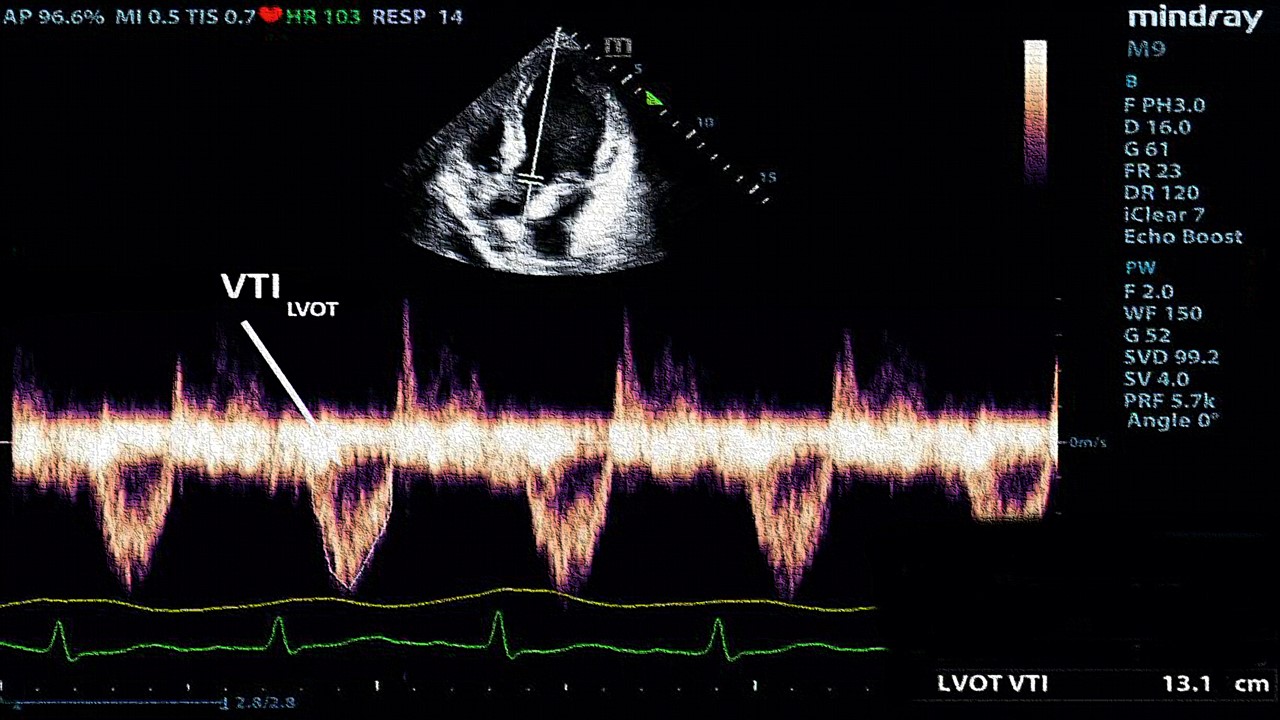
A New Lens on Shock: Hemodynamic Insights Through Critical Care Ultrasound
CCU has transformed the hemodynamic assessment of shock, delivering a reliable, reproducible, and non-invasive tool for ICU clinicians.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.