The Promise of Artificial Intelligence in Breast Cancer
In the field of oncology, where precision medicine is reshaping therapeutic landscapes, artificial intelligence (AI) offers unprecedented potential to refine prognostic tools. Among these, the evaluation of tumor-infiltrating lymphocytes (TILs) in triple-negative breast cancer (TNBC) has emerged as a robust predictor of patient outcomes. While manual TIL scoring by pathologists provides critical insights, it remains constrained by inter-observer variability and subjectivity. The integration of AI-based models promises to overcome these limitations, offering scalable, reproducible, and objective assessment methods.
Tumor-infiltrating lymphocytes are more than immune sentinels; they are biomarkers of the tumor microenvironment’s dynamics and a patient’s intrinsic anti-tumor immunity. Yet, their semi-quantitative evaluation has long been a bottleneck in standardizing care. The advent of AI in computational pathology heralds a new era where deep-learning algorithms can discern patterns beyond human perception, potentially transforming prognostic stratification and clinical decision-making in TNBC.
Decoding the Study: A Comprehensive Approach to AI-Driven TIL Assessment
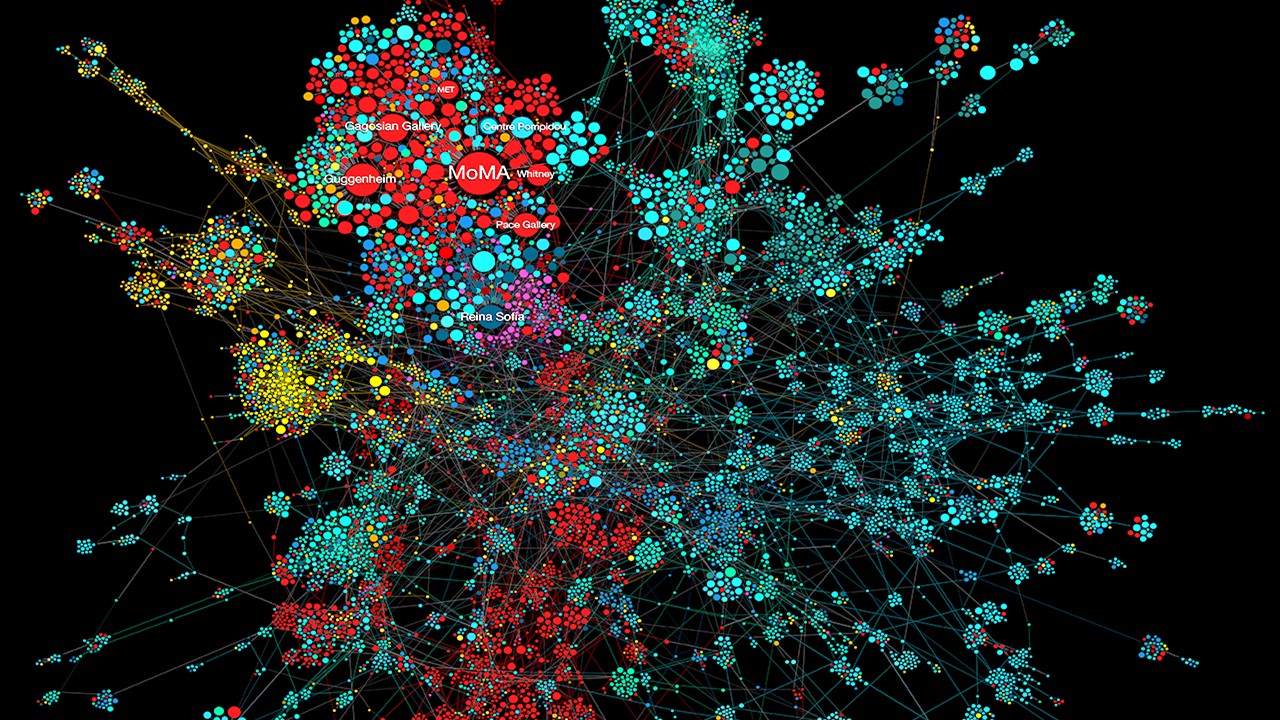
The evaluation of AI-driven TIL assessment models in a recent study provides a granular understanding of their analytical and prognostic validity. This investigation involved ten AI models, each subjected to rigorous internal and external validation against pathologist-read TIL scores. The study was anchored on two robust patient cohorts: an analytical validity cohort from the Yale School of Medicine and a clinical validity cohort from Sweden’s SCAN-B (Sweden Cancerome Analysis Network – Breast) study.
The AI models spanned diverse training methodologies and algorithmic architectures, including K-Nearest Neighbors (KNN), Random Trees (RT), and Neural Networks (NN), along with advanced convolutional neural networks (CNNs) such as HoverNet and CellViT. By juxtaposing these AI-driven models with manual scoring, the study aimed to elucidate not only their correlation with expert assessments but also their predictive prowess for invasive disease-free survival (IDFS).
Analytical Validity: Strengths and Limitations
AI’s ability to replicate and enhance manual TIL assessment was underscored by moderate to high correlations with pathologist-read scores across both cohorts. Notably, models trained on fewer samples, such as RT10, exhibited commendable correlation, rivaling more extensively trained counterparts. This observation reinforces the inherent robustness of TILs as biomarkers of anti-tumor immunity.
However, disparities emerged between internal and external validation sets. The internal cohort demonstrated higher correlations, while external validation revealed performance decrements, reflecting the challenges posed by diverse imaging platforms and patient populations. These findings highlight the need for AI models to undergo rigorous multi-centric validation to ensure generalizability across varied clinical contexts.
Prognostic Validity: AI Models in Predicting Outcomes
The study revealed that eight out of ten AI models demonstrated significant prognostic validity for IDFS in the external cohort. Hazard ratios for these models were comparable and robust, emphasizing their potential to predict clinical outcomes effectively. Interestingly, even models trained on limited datasets retained prognostic accuracy, suggesting that the intrinsic characteristics of TILs as immune markers confer a level of resilience against algorithmic limitations.
Yet, this robustness must be interpreted cautiously. Models trained on small datasets risk overfitting, limiting their applicability in broader clinical settings. The study underscores the imperative for larger, more diverse training datasets to enhance both analytical reliability and prognostic validity.
The CATALINA Challenge: Advancing AI in Pathology
A directly relevant endeavor is the The CATALINA (CollAborative Til vALidatIoN chAllenge) initiative is a pivotal project aimed at evaluating the performance of existing machine learning tools in assessing TILs across multiple phase 3 adjuvant TNBC clinical trials. By focusing on TILs, which are indicative of the immune system’s response to tumors, the challenge seeks to enhance the accuracy and consistency of TIL quantification, thereby improving prognostic assessments and treatment strategies for breast cancer patients.
A key partner in the CATALINA Challenge is the Computational and Integrative Pathology Group (CIPG) from Northwestern University. Renowned for their expertise in developing computational algorithms for TIL assessment, the CIPG brings valuable experience to the project. Their contributions include the creation of large-scale, open-access datasets like BCSS and NuCLS, which contain extensive annotations of tissue regions and cell nuclei in breast cancer. These datasets are instrumental in training and validating deep-learning models for TIL detection, thereby advancing the field of computational pathology. These resources not only enhance the scope of AI training but also ensure that models have exposure to diverse tissue morphologies and immune landscapes, critical for reliable application in heterogeneous patient populations.
The CATALINA Challenge underscores the importance of collaborative efforts in integrating artificial intelligence into pathology. By leveraging machine learning to standardize and automate the evaluation of TILs, the initiative aims to reduce variability in assessments and provide more reliable prognostic information. This endeavor not only enhances diagnostic precision but also paves the way for personalized treatment approaches, ultimately improving patient outcomes in breast cancer care. The initiative exemplifies how partnerships between research institutions and clinical trials can redefine data-driven cancer diagnostics.
Methodological Insights: Beyond Cell Segmentation
The study’s comprehensive analysis illuminated the nuances of various AI methodologies. Cell segmentation-based approaches, such as those employed by HoverNet and CellViT, demonstrated finer granularity, reducing over-segmentation and achieving higher precision. In contrast, patch-based models like Abousamra’s offered an alternative perspective, calculating TIL density over broader tissue regions. While both methods have merits, the choice of approach must align with specific clinical or research objectives.
Deep-learning models such as HoverNet and CellViT exemplify a paradigm shift by enabling simultaneous segmentation and classification. These systems move beyond traditional manual workflows by incorporating phenotypic markers into computational processes. For instance, these models distinguish between immune cells, stromal components, and tumor cells while mapping their spatial organization. This automated interpretation significantly improves the granularity of analysis, offering a more nuanced understanding of the tumor-immune microenvironment (TME). Additionally, these approaches address the inherent subjectivity in manual methods, creating a path toward standardized, reproducible outputs essential for multicentric studies.
Recent advancements have further highlighted the ability of these models to analyze complex spatial relationships within the tissue. By integrating multi-class segmentation with contextual features, these tools capture biologically significant interactions such as immune cell clustering, proximity to tumor margins, and stromal density variations. Such capabilities enrich the prognostic and predictive potential of TILs scoring by emphasizing patterns that manual evaluation may overlook. HoverNet, for example, leverages multi-task learning to refine segmentation accuracy across distinct tissue types, while CellViT employs transformer architectures to account for long-range dependencies in cellular arrangements. These innovations not only enhance the analytical depth of AI models but also align with clinical demands for actionable insights derived from high-resolution histopathological data.
Patch-based models, such as Abousamra’s approach, present an alternative to cell-segmentation methodologies by focusing on classifying entire image patches rather than detecting and segmenting individual cells. This tile-level classification strategy simplifies the computational process, making it particularly effective for broad-scale applications where detailed cell-level resolution is not required. Unlike cell-segmentation models like HoverNet and CellViT, which identify and phenotype individual cells, patch-based models assess regions holistically, identifying areas dominated by lymphocytes or tumor cells. While this reduces the granularity of the analysis, it offers advantages in speed and adaptability to diverse datasets. However, the lack of fine detail in patch-based models can limit their ability to capture nuanced spatial relationships and cellular interactions within the tumor microenvironment. This trade-off highlights a key distinction: cell-segmentation approaches excel in providing detailed insights for complex biological interpretation, while patch-based methods prioritize efficiency and scalability, making them potentially more suited for certain high-throughput clinical applications.
Challenges and the Path Forward
Despite their promise, AI-driven TIL models face significant hurdles before clinical integration. The variability in analytical performance across datasets underscores the need for standardized validation frameworks. Additionally, ensuring transparency in AI decision-making processes is paramount for clinician trust. Cell segmentation-based models offer an advantage in this regard, enabling pathologists to scrutinize individual cell classifications and identify potential errors.
Another critical challenge lies in the accessibility of high-quality, multi-centric datasets. The creation of a global benchmarking platform, akin to the CATALINA challenge, could facilitate the standardized evaluation of AI models while preserving proprietary methodologies.
Transforming Clinical Practice: The Future of AI in Pathology
AI’s role in computational pathology extends beyond TNBC to a broader spectrum of cancers and biomarkers. By providing precise, reproducible assessments, AI tools can complement pathologists, enhancing diagnostic accuracy and prognostic stratification. The integration of these models into clinical workflows will require collaboration among stakeholders, including researchers, clinicians, and regulatory bodies.
As the field advances, AI-driven TIL assessment may become a cornerstone of personalized oncology, guiding therapeutic decisions and monitoring response to treatment. The journey from research to clinical practice is complex, but the potential rewards—a future where every patient receives care tailored to their unique tumor biology—are well worth the effort.
Continuous Cancer Treatment Redefinition
The study of AI-based TIL assessment models illuminates a promising intersection of computational innovation and oncologic care. While challenges remain, the demonstrated analytical and prognostic validity of these models underscores their transformative potential. With continued investment in validation, standardization, and collaboration, AI can redefine how we understand and treat cancer, offering hope for improved outcomes in even the most challenging cases.
Study DOI: https://doi.org/10.1016/j.eclinm.2024.102928
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES

Subscribe
to get our
LATEST NEWS
Related Posts

Immunology & Oncology
The Silent Guardian: How GAS1 Shapes the Landscape of Metastatic Melanoma
GAS1’s discovery represents a beacon of hope in the fight against metastatic disease.
Immunology & Oncology
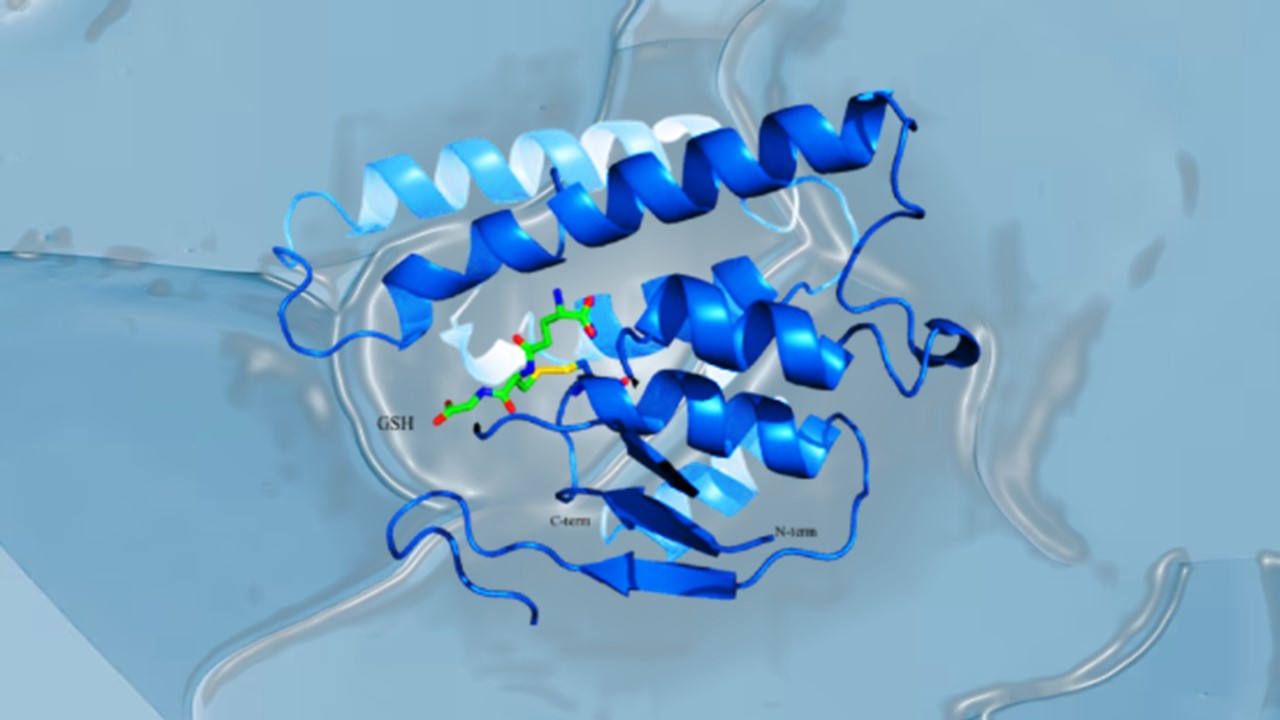
Resistance Mechanisms Unveiled: The Role of Glutathione S-Transferase in Cancer Therapy Failures
Understanding this dual role of GSTs as both protectors and accomplices to malignancies is central to tackling drug resistance.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.
Designing Better Sugar Stoppers: Engineering Selective α-Glucosidase Inhibitors via Fragment-Based Dynamic Chemistry
One of the most pressing challenges in anti-diabetic therapy is reducing the unpleasant and often debilitating gastrointestinal side effects that accompany α-amylase inhibition.