Obesity is defined as the medical condition whereby an individual accumulates body fat to the point where their health is impacted. It is often not thought of as a disease in the pathological sense – but it is undeniably a risk factor for a myriad of other diseases. Over 42% of Americans are classified as obese, while the global medical cost of obesity is estimated to account for $990 billion. Despite the growing burden of the condition on a worldwide scale – with the global prevalence of obesity having tripled between 1975 and 2016, pharmacological responses remain few, although growing.
Defining Obesity
While obesity may be commonly understood to mean the excess depositing of fat in the body, the actual medical definition may be more complex – particularly when trying to translate this to something that can be used as a quick descriptor. Body Mass Index (BMI) is often used – with a BMI greater than 30 often being used as the cut-off point for obesity. BMI cut-offs are commonly adjusted for racial minorities, according to the risk of developing Type 2 Diabetes in their demographic.
But this definition does not account for the other risks that come with obesity, nor does it elucidate any mechanistic links between obesity and the dangers it comes with. Obesity has been linked to higher levels of overall inflammation in the body. Inflammation itself has been linked to numerous other health risks: higher insulin resistance (and therefore higher insulin levels) and higher levels of estrogen. The metabolic effects of obesity are also widespread; but in the scope of this article it is more pertinent to appreciate that the causative links between obesity and its consequential diseases are complex – rather than to pinpoint all of them.
Risks associated with Obesity
The consequences of obesity are manifold and well-documented. Associated comorbidities include Type 2 Diabetes, Cardiovascular Disease and an increased risk of a plethora of cancers. Other risks are also corollary to these – such as hypertension, cholesterol imbalances and gallbladder diseases. Additionally, obesity may cause sleep apnea, breathing problems and osteoarthritis. The list of these conditions already includes some of the leading causes of mortality – particularly in the developed world.
Many of the conditions that are reinforced by obesity cause positive, reciprocal feedback loops which results in each disease increasing the risk or severity of the other. A particularly well-established reciprocal link lies between obesity and depression: depression may give rise to unhealthy weight gain or lack of exercise, while an elevated state of inflammation (which is caused by weight gain) may give rise to depression.
Furthermore, one could not discuss the comorbidities of obesity without addressing the elephant in the room: the current pandemic. Obesity has been classified as one of the leading risk factors for the development of severe disease; a BMI above 30 has been associated with a +40% risk of dying of COVID-19, with the risk increasing higher as BMI does. It is estimated that this may be due to obesity leading to higher levels of insulin and inflammation in the body, with higher levels of cytokines, and lower levels of adinopectin.
Perspective of Obesity
A particular flaw, on a societal and institutional level, is to view obesity as non-clinical. Particularly throughout the pandemic, much discourse relating to comorbidities for COVID-19 has labelled obesity as one of the leading preventable causes of death due to the coronavirus. This belies the deeply ingrained prejudice to blame individuals for their obesity: but any number of conditions which are also risk factors for COVID could also be called “preventable” yet the same language is not used in discussions revolving around such circumstances.
Such institutional bias is evident in comparing the tone and language used by the British NHS for obesity: language that is often alarmist, patient-blaming and highlighting the need to reduce costs associated with obesity. But this is not the way other diseases with growing burdens are treated – conditions which often receive growing budgets and levels of care. Indeed, in the UK All-Party Parliamentary Group on Obesity’s 2020 report, only “26% of people with obesity reported being treated with dignity and respect by healthcare professionals when seeking advice or treatment for their obesity”.
This is further reflected in how the American Medicare Social Security Act does not authorise insurance coverage of obesity or related illnesses, although the Treat and Reduce Obesity Act promises to change that. As obesity is a condition with variable genetic, epigenetic, societal and environmental factors, it is important that the condition be treated on a clinical level with the appropriate manner of humane attention moving forward.
Medical Interventions
Another result of the long-embedded view of obesity as a lifestyle problem rather than the multifaceted disorder is the dearth of available pharmaceutical solutions for the condition, despite the growing market and demand for treatment.
Current Treatments include
- Orlistat: One of the most widespread medications for treating obesity, with clear but only moderate results – with a study showing mean loss of ~10.6kg and a ~37% risk reduction for Diabetes. It works by inhibiting lipase enzymes and reducing the absorption of fats, which also comes with the side-effects of oily stool and related disturbances.
- Liraglutide: As a glucagon-like peptide-1 receptor agonist which mimics the function of the incretins (hormones which reduce the level of sugars in the blood), it works by increasing the levels of insulin and reducing the amount of glucagon produced. A study found >76% of participants on liraglutide lost ≥5% of their starting weight, compared to placebo (30%) or orlistat (44%); additionally, over three-quarters of participants showed a reduction in prediabetes. However, liraglutide also comes with a host of possible side-effects including cancer, pancreatitis, kidney problems and gallbladder disease.
- Lorcaserin: Lorcaserin possesses serotonergic properties, activating brain receptors in the hypothalamus; despite promising results prior to its FDA approval in 2012, it was withdrawn from the market in 2020 after observational studies associated it with a higher risk of cancer.
- Phentermine/topiramate: Often used in combination therapies, these two substances have known appetite suppressing or weight lessening effects, although their exact mechanism of action remains unknown. A review carried out on hypertensive patients found that phentermine/topiramate caused more significant weight loss than orlistat, as well as lowering blood pressure. Despite receiving FDA approval, it has not received approval by the EMA – citing a range of circulatory side-effects
- Naltrexone/bupropion: This combination of drugs is hypothesised to suppress hunger centers in the brain, though their exact mode of action is unclear. Phase III trials indicated -6.1% change in body weight, although only 50% of participants completed the trials due to significant side effects including constipation, nausea and headaches.
The safety profile of anti-obesity medication has remained an evergreen issue in the area, with over 25 substances withdrawn from the market between 1964 and 2009 over concerns regarding their adverse effects.
Ways Forward
As such, it becomes obvious that pharmacological interventions for obesity have so far only provided modest gains at the expense of significant adverse events. Developed by Novo Nordisk Semaglutide was approved in 2021 by the FDA and was found to be associated with sustained weight loss, with an average -15.6kg change in body weight over 68 weeks (compared to a -2.6kg change in the trial’s placebo group). Its improved safety profile is in part due to its injectable nature, which eliminates the need to ingest it on an empty stomach, although it still carries significant side effects. Another study which surveyed the effects of semaglutide in combination with cagrilintide found even more promising results, with participants losing 17% of their original weight, compared to 7% for those only on semaglutide.
While bariatric surgery remains the most effective way to tackle severe obesity, it is wildly expensive and time-consuming – and it can have long-lasting effects and the usual adverse reactions associated with any form of surgery (particularly if incisions are required). A cursory look at the numbers of afflicted people worldwide would quickly reveal the infeasibility of relying on surgery. Despite the rocky road that anti-obesity pharmacological solutions have had to endure – particularly regarding safety, the demand for assistance in shedding weight is only expected to grow; innovations that can improve on efficacy and safety will no doubt be groundbreaking.
Nick Zoukas, Former Editor, PharmaFEATURES
Subscribe
to get our
LATEST NEWS
Related Posts

Chronic & Debilitating Diseases
Renopathology Tipping Point: Deciphering the Molecular Code of Stage 2 Chronic Kidney Disease
The molecular events of Stage 2 CKD, from inflammation to lipid metabolism, offer insights for diagnosis and treatment.
Chronic & Debilitating Diseases
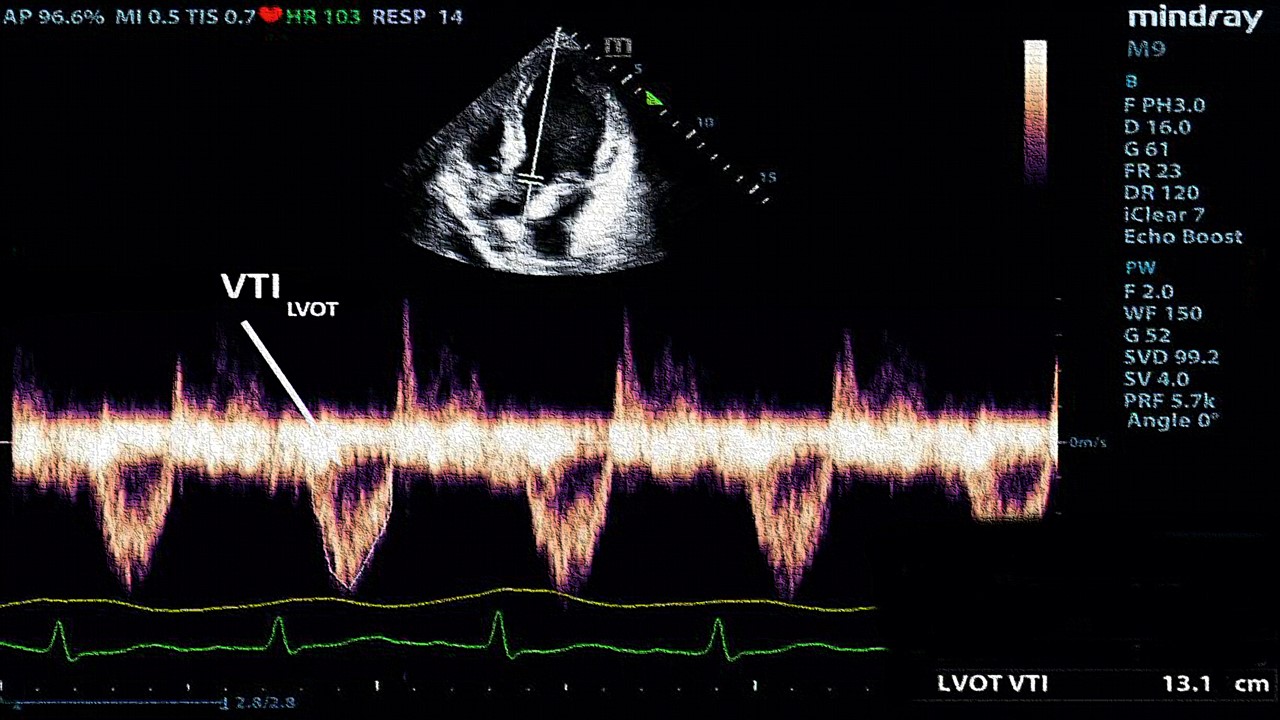
A New Lens on Shock: Hemodynamic Insights Through Critical Care Ultrasound
CCU has transformed the hemodynamic assessment of shock, delivering a reliable, reproducible, and non-invasive tool for ICU clinicians.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.