Developing minimally invasive, accurate cancer screening tests has been a strong focus for cancer research in recent years. An increasing number of studies have highlighted the potential of circulating tumor DNA as a potential candidate for both diagnostic and prognostic value. While research is ongoing to investigate this potential biomarker, recent advancements like the Galleri blood test show how far precision oncology has come.
Introduction
Circulating cell-free DNA (cfDNA) is a type of DNA detectable in the plasma and serum of healthy individuals as a result of programmed cell death, known as apoptosis. Cancer patients typically show a higher amount of cfDNA, as tumour cells divide more rapidly than normal cells. The proportion of cfDNA derived from a tumour is indicated as circulating tumour DNA (ctDNA).
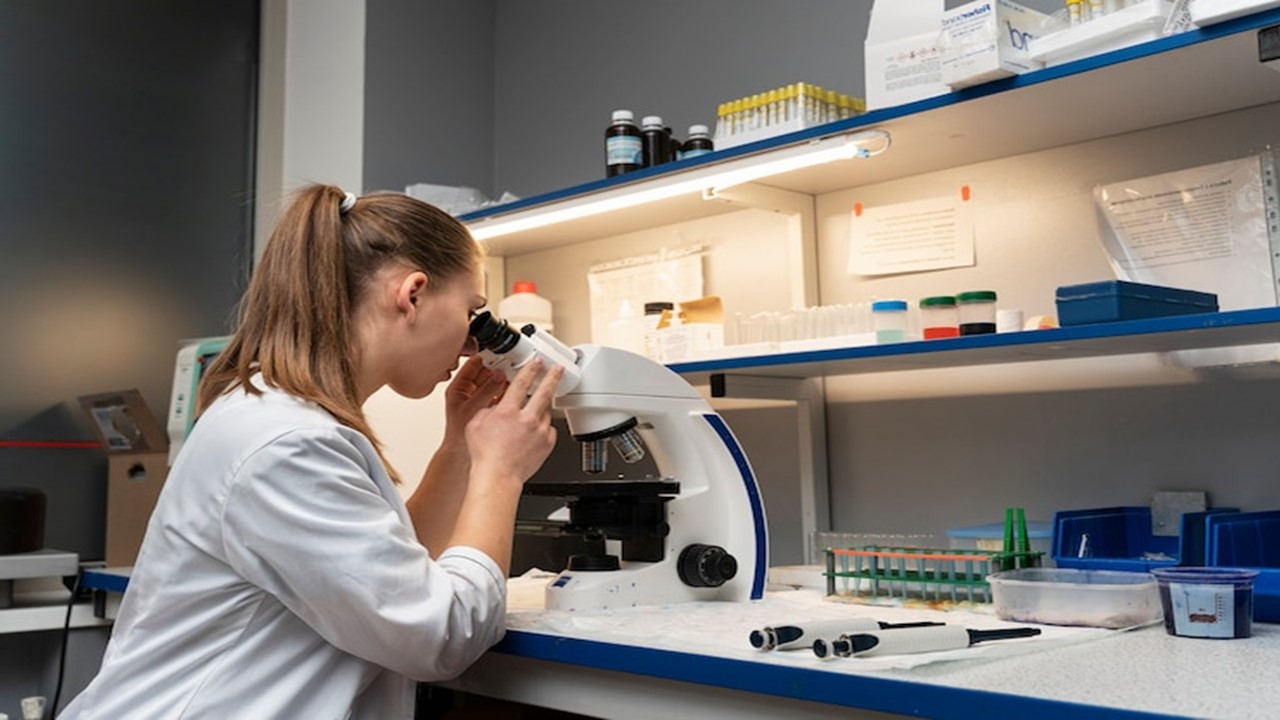
Currently, cfDNA extraction is performed using columns or magnetic beads, a phenol-chloroform-based method, and a filtration-based method – a number of extraction kits are available on the market.
In recent years, analysis of both cfDNA and ctDNA has been under the limelight as potential blood biomarkers. Both have demonstrated predictive and prognostic value, but research is ongoing to refine this technique to optimise the accuracy of cancer detection.
The impact of this research has led to the development of liquid biopsies, a next-generation sequencing (NGS) technique which analyses ctDNA from blood and plasma. This technique is particularly attractive because of the minimally invasive method of capturing tumour-specific genomic alterations in circulation.
Initially PCR-based methods were used to sequence ctDNA due to their sensitivity and low cost. However, these methods can only screen for known variants, and the input and speed are limited. NGS has shown to provide high throughput and the ability to screen unknown genetic variants. Thanks to NGS technology, the sequencing of ctDNA can be performed at a much higher sensitivity than tissue biopsies and support patients in targeted therapy relative to their tumour profile.
In August 2020, the FDA approved the first liquid biopsy companion diagnostic – Guardant360 CDx assay. According to an FDA press release, this test uses NGS to recognise patients which present specific mutations of the epidermal growth factor gene. This specific type of mutation is expressed in a deadly form of metastatic non-small lung cancer. It is the first approval for NGS and liquid biopsy in one diagnostic test.
Precision oncology capabilities
Cancer screening and monitoring
The two main methods of detecting ctDNA are droplet digital polymerase chain reaction (ddPCR) and highly-sensitive NGS. NGS is a DNA-sequencing technique which can sequence the entire human genome in a day. According to a review, “each of the three billion bases in the human genome is sequenced multiple times, providing high depth to deliver accurate data and an insight into unexpected DNA variation”. In one test, NGS allowed clinicians to detect mutations in 55 tumorous genes, instead of assessing one gene at a time.
The correlation between ctDNA and presence of cancerous regions has pushed researchers to investigate the diagnostic capabilities of blood tests which detect this genetic material. The vast majority of research investigating the potential use of ctDNA is focused on the detection of specific mutations detected in the plasma/serum of cancer patients.
It has been suggested that if researchers assume all regions of the tumor secrete ctDNA at the same rate, “sequencing the genetic material will provide a far more comprehensive overview of all the mutations present in the tumor than just sequencing small lesions”.
Liquid biopsy has been investigated as an attractive alternative to solid (tissue) biopsies for a while, potentially overcoming limitations such as sampling bias and difficulty in repetitive sample extraction.
In addition, due to the short half-life of circulating DNA, genetic analysis could demonstrate “real time” insights into the mutations that arise during therapy. This is due to the fact that ctDNA typically accounts for less than 1% of the total cfDNA. Of course, this presents a challenge as the material degrades so quickly, hence research is currently investigating the feasibility of automated methods of ctDNA analysis.
Prognostic biomarker
Other researchers are investigating the prognostic value of ctDNA biomarkers, in order to gage an idea of the risk for relapse and metastasis.
A 2021 paper recently published, highlights the findings of a clinical trial investigating the detection and clinical value of circulating tumor cells as an assisted prognostic marker in colorectal cancer patients.
The data indicated that with increased tumor stage, the number of ctDNA also increased, with significant statistical differences. In addition, detection of serum biomarkers in ctDNA-positive and ctDNA-negative groups indicated a significantly increasing expression in the CTC-positive group.
In terms of prognostic value, it was inferred that the sensitivity of ctDNA could be related to lymphatic metastasis, and the depth of filtration. Monitoring of the ctDNA levels could be a useful tool in assessing the clinical staging and estimating the prognosis of patients based on ctDNA as a biomarker.
Latest advancements – The Galleri blood test
A potential breakthrough in cancer screening is making its way onto the NHS, offering hope for thousands of cancer patients in the UK. More than 100,000 volunteers aged between 50 and 77 are being sought to provide blood samples at mobile clinics across England to assess how well the Galleri test works in the health service.
Results from the latest studies into Galleri so far have been promising. According to Cancer Research UK, the “GRAIL reports that the test can detect 50 different types of cancer with a false positive rate of 0.5%. This means that in approximately 200 people tested, 1 person would be expected to receive a positive result when they do not have cancer.” The blood test, similar to liquid biopsies, detects and sequences cfDNA in circulation.
Up until now, the test has only been trialled in patients already diagnosed with cancer. However, the NHS is hoping to test the sensitivity of the blood test in a much larger sample of individuals without cancer diagnosis. The outcome of the clinical trial is to determine whether the test can reliably detect cancer at the earlier stages. If successful, this would be a huge achievement for cancer research, and could potentially save thousands of lives by intervening with treatment earlier than if diagnosed at a later stage.
In addition, it could even reduce the need for tissue biopsies which are more invasive and cannot be conducted as frequently, which can be a problem for disease monitoring.
It will take time to determine the accuracy and reliability of this blood test, and a number of other tests for different mediums are in development. It is however promising to see the direction for precision oncology in terms of tailored treatment for disease type and progression.
Charlotte Di Salvo, Editor & Lead Medical Writer
PharmaFeatures
Subscribe
to get our
LATEST NEWS
Related Posts
Precision Medicine
PrecisionLife and Nanopharmaceutics Join Forces to Advance Precision Medicine for CNS Disorders
Combinatorial analytics and nanoscience – perfect combination!
Precision Medicine
Unleashing Precision Medicine: Engineered Phages for E. coli Treatment
Hemo-oncology prognosis is shown to improve along with marked E. coli associated morbidity and mortality reduction with a newly developed Phase 1 drug candidate.
Read More Articles
Synthetic Chemistry’s Potential in Deciphering Antimicrobial Peptides
The saga of antimicrobial peptides unfolds as a testament to scientific ingenuity and therapeutic resilience.