Unveiling Metastasis Suppressors: Cracking the Code of Cancer Spread
Metastasis suppressor genes represent a unique class of genetic regulators that selectively inhibit the dissemination of cancer cells to distant organs without influencing the primary tumor’s growth. This distinction makes them pivotal in understanding and combating metastatic progression, the primary cause of cancer-related mortality. The complexity of metastasis—spanning invasion, circulation, survival in hostile environments, and colonization at secondary sites—has historically hampered efforts to identify these genes systematically. However, recent breakthroughs in genomic tools, including RNA interference (RNAi)—a method of silencing gene expression through small RNA molecules—and three-dimensional (3D) culture systems, have transformed the landscape of metastasis research.
Unlike traditional cancer drivers, metastasis suppressors act at bottleneck stages of the metastatic cascade, preventing malignant cells from overcoming critical barriers. Their role extends beyond simply halting physical dissemination; they influence survival pathways, microenvironment interactions, and cellular adhesion dynamics, forming an intricate defense system against metastatic progression. Despite their importance, relatively few metastasis suppressor genes have been identified due to the lack of experimental systems capable of isolating these unique genetic functions effectively.
The genome-wide short hairpin RNA (shRNA) screening approach used in the discovery of GAS1 (Growth Arrest-Specific 1) exemplifies the evolution of metastasis research. By leveraging a library targeting tens of thousands of genes, researchers developed a method to mimic key metastatic steps ex vivo (outside a living organism), bridging the gap between in vitro (test tube or culture dish) simplicity and in vivo (inside a living organism) complexity. This strategy not only confirmed the existence of known suppressors but also uncovered novel candidates like GAS1, advancing our understanding of metastasis from an abstract process to a molecularly defined pathway.
Innovative Methodologies: The Science of Finding Hidden Genes
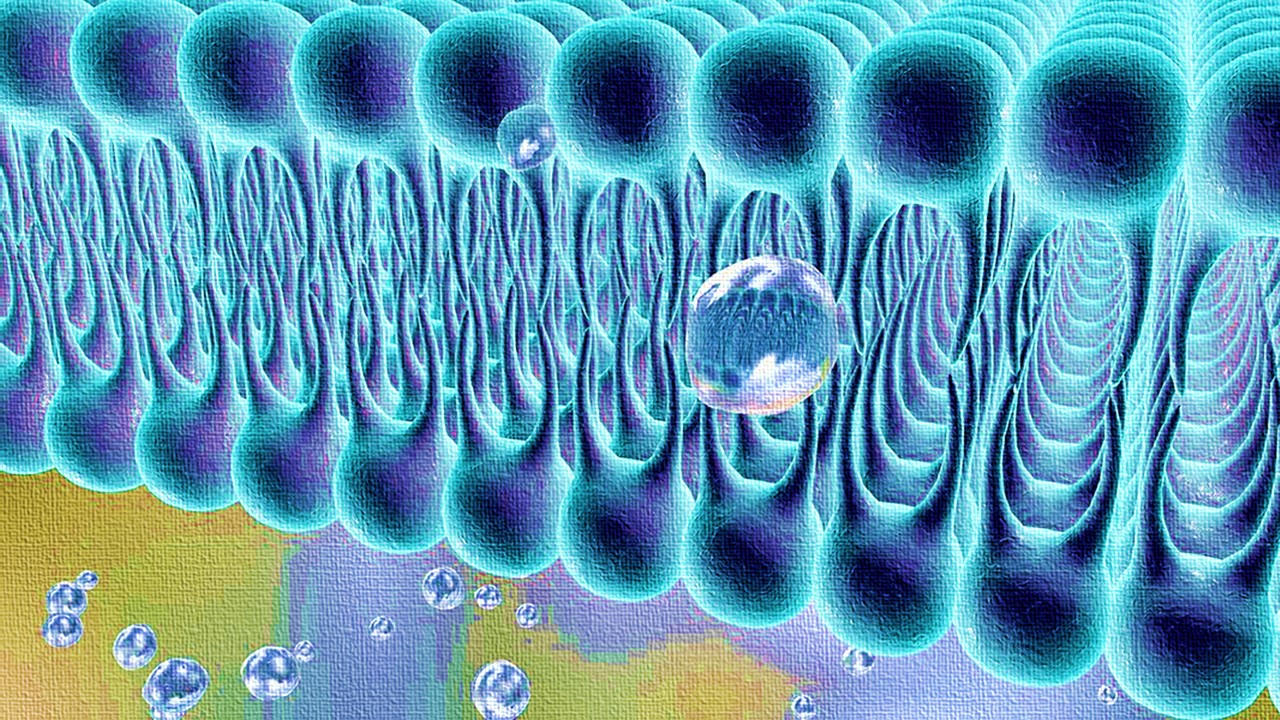
To dissect the molecular intricacies of metastasis, researchers relied on a three-dimensional (3D) cell culture system, an advanced platform replicating the extracellular matrix (ECM)—the network of proteins and molecules that provides structural and biochemical support to surrounding cells. Unlike conventional two-dimensional (2D) assays, 3D cultures simulate real-world tumor behaviors, including cell invasion, motility, and colonization. In this context, weakly metastatic B16-F0 mouse melanoma cells were embedded in collagen and fibrin matrices to assess their ability to form satellite colonies—a hallmark of metastatic potential.
The integration of a genome-wide short hairpin RNA (shRNA) library with this 3D platform was groundbreaking. Each shRNA targeted a specific gene, silencing its expression in B16-F0 cells. The researchers observed that knockdown of certain genes led to increased satellite colony formation, indicating a loss of metastatic suppression. Among 78 initial candidates, 22 genes emerged as suppressors, displaying the ability to limit metastasis in secondary site models without affecting primary tumor growth. This non-biased screening illuminated the molecular nodes critical to metastatic regulation, paving the way for therapeutic interventions.
The validation process was equally rigorous. Candidate genes underwent secondary screenings, mouse tail vein injection assays, and spontaneous metastasis models to confirm their roles. These complementary approaches ensured that only genes directly influencing metastasis—such as GAS1—were prioritized. This methodology exemplifies the precision required to unravel metastasis’s complexity, providing a robust framework for identifying suppressors across diverse cancer types.
GAS1: A Sentinel Against Melanoma Metastasis
GAS1 (Growth Arrest-Specific 1) emerged as a key player in suppressing melanoma metastasis, distinguished by its ability to inhibit metastatic colonization while leaving primary tumor growth unaffected. This glycosylphosphatidylinositol (GPI)-anchored membrane protein displayed a significant expression disparity between poorly metastatic B16-F0 cells and their highly metastatic counterparts, B16-F10. Notably, down-regulation of GAS1 in B16-F10 cells correlated with their enhanced metastatic capability, suggesting a causal relationship. Reintroducing GAS1 into these aggressive cells reversed their metastatic behavior, reducing satellite colony formation in 3D cultures and lung metastases in vivo.
The role of GAS1 extends beyond mere presence; its functional impact lies in promoting apoptosis—a form of programmed cell death—at secondary sites. Metastatic melanoma cells often evade programmed cell death, a critical survival mechanism during dissemination. GAS1 counters this evasion, fostering apoptosis upon cell arrival at distant tissues, thereby limiting their colonization ability. Interestingly, this pro-apoptotic role does not interfere with primary tumor dynamics, making GAS1 a specific guardian of metastatic barriers.
Ectopic expression studies further validated GAS1’s suppressive potential. By artificially increasing GAS1 levels in metastatic models, researchers demonstrated a marked reduction in metastatic lesions without any compromise to primary tumor integrity. These findings highlight GAS1’s precise and targeted functionality, positioning it as a promising candidate for therapeutic development in melanoma and beyond.
Mechanistic Insights: How GAS1 Promotes Apoptosis
The primary mechanism by which GAS1 suppresses metastasis lies in its ability to enhance apoptosis, particularly after cancer cells reach secondary sites. Upon arrival in the lungs, melanoma cells with reduced GAS1 expression exhibited prolonged survival and decreased apoptotic signaling. Quantitative imaging revealed that while initial cell numbers in the lungs were comparable between GAS1-deficient and control cells, GAS1 knockdown significantly increased cell persistence over time. This survival advantage was accompanied by diminished activation of caspase pathways, a cornerstone of apoptotic regulation.
Further analysis connected GAS1’s activity to its interaction with survival signaling pathways. Preliminary data suggest that GAS1 might modulate receptor tyrosine kinase (RTK) signaling, particularly through Ret (Rearranged during Transfection), to influence apoptotic thresholds. However, its precise molecular targets remain elusive. Interestingly, GAS1’s role in apoptosis aligns with other metastasis suppressors, such as Caspase 8 and BRMS1 (Breast Cancer Metastasis Suppressor 1), which similarly prevent metastatic colonization by enhancing programmed cell death. This functional convergence underscores apoptosis as a critical checkpoint in metastasis suppression.
Experimental models bolstered these findings. Overexpression of anti-apoptotic proteins like Bcl-2 (B-cell lymphoma 2) mimicked the effects of GAS1 knockdown, reinforcing the link between apoptosis and metastatic restraint. These insights not only clarify GAS1’s biological role but also highlight potential therapeutic strategies, such as mimicking its apoptotic effects or restoring its expression in metastatic cells.
Clinical Relevance: GAS1 in Human Melanoma
The significance of GAS1 extends beyond experimental models, finding resonance in human melanoma biology. Analysis of patient samples revealed that GAS1 expression was consistently lower in metastatic melanomas compared to primary tumors. Tissue microarray studies showed that while over 80% of primary melanomas expressed detectable levels of GAS1, fewer than half of metastatic samples did. This stark contrast underscores the role of GAS1 down-regulation as a hallmark of metastatic progression.
Cell line studies mirrored these trends. Human melanoma lines derived from primary tumors exhibited high GAS1 expression, whereas those from metastatic sites displayed marked reductions. Functional assays demonstrated that reintroducing GAS1 into these metastatic cell lines reduced their ability to form satellite colonies, validating its suppressive role in human cancer. These findings position GAS1 as both a biomarker for metastatic potential and a potential therapeutic target.
Publicly available genomic datasets further supported these observations, revealing significant GAS1 down-regulation in metastatic samples across multiple melanoma cohorts. This cross-validation across independent datasets solidifies GAS1’s relevance in human disease, marking it as a focal point for future melanoma research and treatment strategies.
Expanding Horizons: GAS1 Beyond Melanoma
Although initially studied in melanoma, GAS1’s influence appears to extend to other cancer types. Data from breast and prostate cancer models indicate that GAS1 down-regulation is not melanoma-specific but a broader feature of metastatic progression. In mouse breast cancer models, GAS1 knockdown enhanced lung colonization, mirroring its effects in melanoma. Similarly, prostate cancer samples showed a clear correlation between GAS1 suppression and advanced disease stages.
The versatility of GAS1 as a metastasis suppressor highlights its potential as a universal therapeutic target. Restoring GAS1 expression or mimicking its function could serve as a common strategy for tackling metastasis across cancer types. Understanding the regulatory mechanisms behind GAS1 down-regulation, including epigenetic silencing or transcriptional repression, will be crucial in translating these findings into clinical applications.
Furthermore, GAS1’s ability to interact with diverse signaling pathways opens avenues for combination therapies. By targeting GAS1 alongside other metastatic regulators, researchers could develop synergistic approaches to halt cancer spread. These broader implications emphasize the importance of GAS1 not just as a melanoma suppressor but as a cornerstone in metastasis research.
The Road Ahead: Implications for Cancer Treatment
The discovery of GAS1 as a metastasis suppressor marks a transformative step in oncology, highlighting the potential to intervene in metastatic progression with precision. While the field has traditionally focused on halting primary tumor growth, GAS1 shifts attention to the downstream processes that drive cancer lethality. By elucidating its apoptotic mechanisms, researchers can develop therapies that specifically target metastatic cells without affecting healthy tissues or primary tumor dynamics.
However, the path to clinical application is not without challenges. Identifying the molecular triggers for GAS1 down-regulation and overcoming them will require sophisticated genomic and pharmacological tools. Additionally, translating findings from preclinical models to human therapies necessitates careful validation and optimization.
Despite these hurdles, GAS1’s discovery represents a beacon of hope in the fight against metastatic disease. As researchers continue to unravel its complexities, GAS1 could redefine cancer treatment, offering new strategies to transform a once-terminal diagnosis into a manageable condition.
Study DOI: https://doi.org/10.1101/gad.1714608
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES
Subscribe
to get our
LATEST NEWS
Related Posts

Immunology & Oncology
Resistance Mechanisms Unveiled: The Role of Glutathione S-Transferase in Cancer Therapy Failures
Understanding this dual role of GSTs as both protectors and accomplices to malignancies is central to tackling drug resistance.

Immunology & Oncology
An Oncological Breakthrough: Envonalkib Outperforms Crizotinib in Treating ALK-Positive Lung Cancer
Genetic and environmental factors affecting NSCLC progression and treatment response necessitate global validation of these envonalkib trial findings.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.