Malaria continues to be one of the leading contributing factors to the global burden of disease – with 241 million new cases in 2020, and 627,000 deaths. Much of the burden of malaria lies in Sub-Saharan Africa, where the disease is highly widespread. Investing in ways to tackle the disease in the area is central to the World Health Organization’s (WHO) Malaria strategy, which aims to reduce incidence of the disease by 90% before 2030. However, the developed world should take caution: with increasing global warming, the vectors for malaria are set to expand their range farther towards Europe. Solving the ongoing malaria crisis should thus be a global priority.
Understanding Malaria
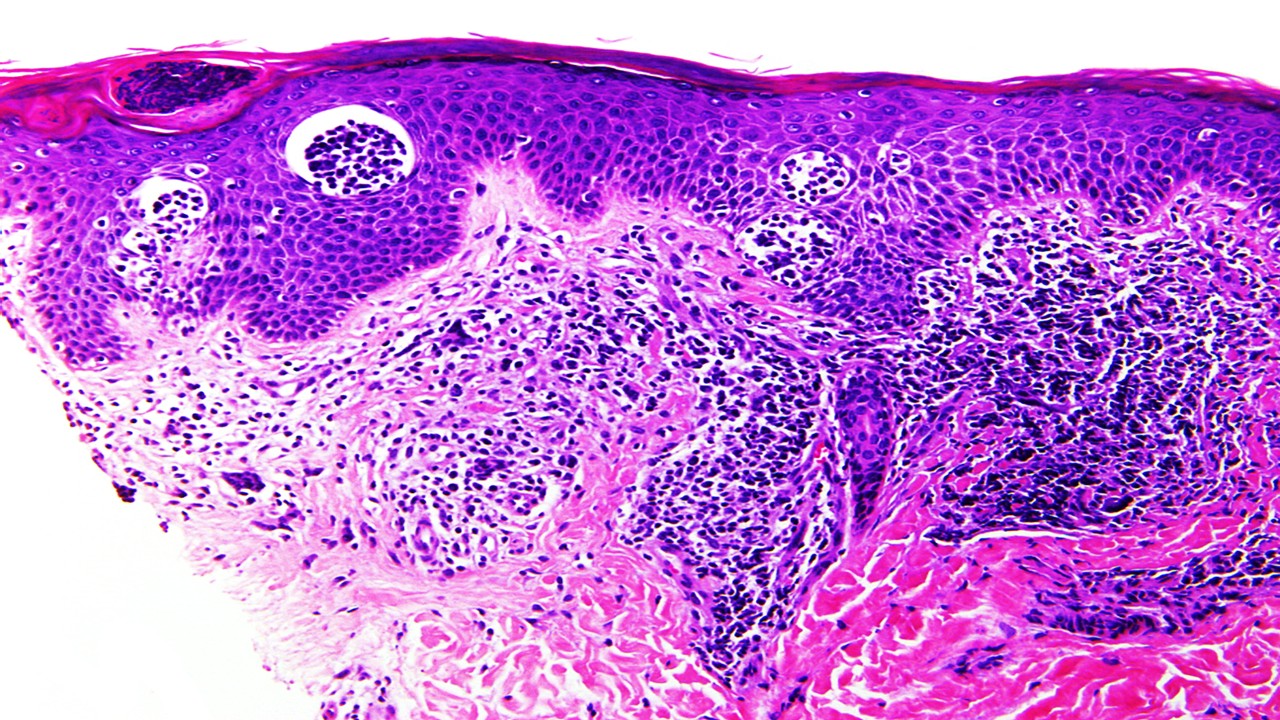
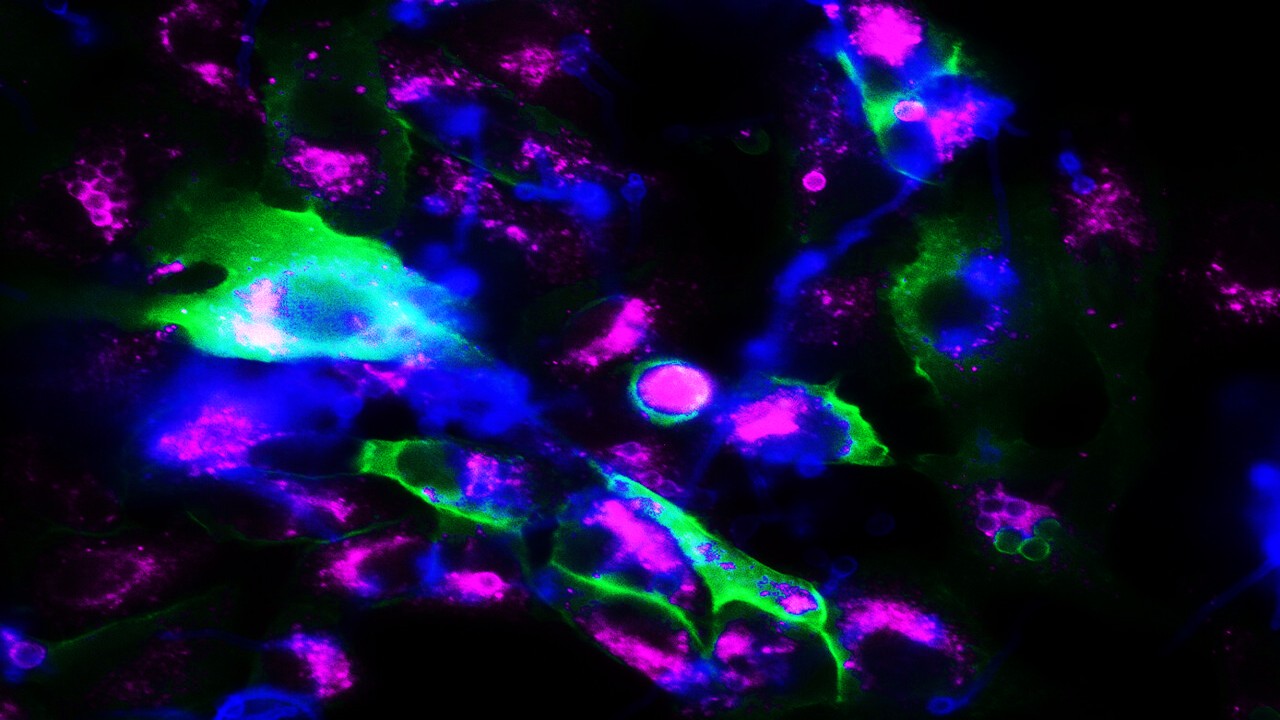
Malaria is caused by six protozoan organisms from the Plasmodium genus. Plasmodium falciparum is the leading species responsible for disease (~75% of cases), with Plasmodium vivax the second most common species (~20% of cases). Plasmodium protozans are obligate parasites, with a life-cycle involving multiple hosts. They grow in insects, usually mosquitoes of the Anopheles genus, which function as vectors that transport them to mammals. Once they find their way to mammals, they mature in host tissue – usually the liver, before infecting red blood cells from which new vector mosquitoes can pick them up and continue their life cycle. It is this infection of red blood cells that is responsible for most symptoms associated with malarial disease – and it is the range of the Anopheles mosquito which limits the area which malaria can occur in.
Preventing Malaria
The most cost-efficient route towards eliminating malaria has always been prevention, rather than treatment. The persistence of malaria in any geographical region requires high densities of human and Anopheles populations, as well as high transmission rates between these two populations. Eliminating any of these can result in the local eradication of indigenous cases – as we have seen in North America, Europe and the Middle East. However, elimination of the disease still requires significant upfront investments. This is in stark contrast to controlling the disease and maintaining low rates of endemicity rather than complete elimination. However, the cost of implementing preventative measures can vary widely between countries – and it is this cost that is the chief determinant of whether elimination will be cost-saving compared to control. Its reliance on volatile, unpredictable sources such as national governments, or foreign donors, further complicates the planning of a robust, long-term strategy.
Beyond traditional prevention measures such as mesh nets, and ways to limit mosquito exposure, 2021 has seen the approval of the first vaccine for malaria: Mosquirix. While studies investigating the efficacy of the vaccine have found only modest benefit, its preventative value is significant when examined on a public health scale. Estimates indicate that for every 100,000 children receiving 4 doses of the jab, 116,480 cases of malaria and 484 deaths are prevented in high-transmission areas. The cost-benefit ratio of the vaccine is comparable to other preventative strategies when a cost of $5 per dose is assumed. Future vaccines will no doubt improve upon these points, with hopes of vaccination playing a key role in elimination.
Treatment and Its Role in Malaria
The WHO’s E-2020 initiative has already seen 8 countries out of 21 reporting zero indigenous malaria cases, a remarkable achievement. However, only 2 out of 21 countries in the initiative are from Sub-Saharan Africa – which remains the most challenging region. Antimalarial treatments remain critical for treating malaria, but also for chemoprophylaxis. Chemoprophylaxis refers to the practice of administering antimalarials to prevent infection – which is effective, although costly. Quinine was the first anti-malarial agent – and many derivatives of the compound soon followed, with chloroquine being the most widely used and cost-effective agent. However, chloroquine faces increasing drug resistance – especially when used outside of combination therapies. Other treatments include artemisinin and its own derivatives, as well as multiple repurposed antibiotics which have shown antimalarial activity, such as doxycycline.
Developing new classes of drugs for malaria remains challenging however, particularly due to the disproportionate burden of malaria in poorer countries. This makes the endeavor of antimalarial innovation less attractive for industrial actors, and much of the research is led by academia. Given the increase in drug resistance over the last decade, the need for new agents remains dire. However, new target-driven drug discovery approaches have yielded promise for future efforts. This is complemented by cheaper, far more cost-effective drug repurposing approaches – such as the demonstration of antimalarial activity in methylene blue, fosmidomycin, and others.
Climate Changing and Malaria: An Infectious Duo
In a scenario where global temperatures rise only by 1℃ until 2100, an additional 2.4 billion people are expected to be at risk of malaria due to climate change. A global increase of 1℃ is largely accepted as non-viable anymore however, with 1.5℃ considered ambitious in itself. Under worse conditions, with a 3.7℃ increase by 2100, an additional 4.7 billion people will be at high risk of malaria. As temperatures rise, areas farther from the equator become hospitable to Anopheles mosquitoes which can carry the disease. This also increases the risk for other diseases vectored by mosquitoes – including Dengue fever. This includes areas throughout continental Europe and most of the United States – which were previously regularly exposed to malaria up until the early 20th century, prior to interventions for its elimination.
Future Outlooks
Heightening our efforts against malaria will be to the benefit of the entire planet. The impact of malaria is not only evident in the high burden of disease it presents year after year, but it is also imprinted on the human genome. Some of the most common hereditary diseases have evolved to make human red blood cells far less hospitable to Falciparum infection: these include thalassemia, sickle-cell disease and glucose-6-phosphatase deficiency. The prevalence of these conditions largely coincides with the historical range of Anopheles mosquitoes, including around the entire Mediterranean basin – a reminder of how close the disease can come if left unchecked.
The fight to end malaria must continue – and the WHO’s goals for limiting the disease present worthy goals for global health, social justice and safety. Malaria, along with other infectious diseases and their excessive economic burden, account for a substantial limiting factor in the growth of Sub-Saharan Africa, Southeast Asia and South America. As the COVID-19 pandemic presents us with a more aware and health-literate population, the time is opportune to raise awareness for the global strategy to eliminate malaria – and why it should matter for all of us.
Nick Zoukas, Former Editor, PharmaFEATURES
Subscribe
to get our
LATEST NEWS
Related Posts

Infectious Diseases & Vaccinology
Enduring Blockade: Five-Year Functional Antibody Persistence Against Emerging GII.4 and GII.17 Noroviruses
Natural infection with dominant GII noroviruses elicits long-lived functional antibodies, redefining immune durability in viral gastroenteritis.
Infectious Diseases & Vaccinology
Resistant Mycosis: Reimagining Antifungal Therapy Through Mechanistic Innovation and Molecular Disruption
Emerging antifungal strategies are redefining treatment by targeting fungal physiology through diversified, mechanism-driven approaches that overcome entrenched drug resistance.
Infectious Diseases & Vaccinology
Fungal Refractory States: Deciphering Pathobiology and Therapeutic Weaknesses in the Era of Rising Antifungal Resistance
Rising antifungal resistance reflects a multidimensional biological challenge that demands mechanistically innovative, host-integrated therapeutic strategies.

Infectious Diseases & Vaccinology
Epigenetic Parasite Vulnerabilities: Repurposing Histone Deacetylase Inhibitors for Complex Multispecies Therapeutics
Repurposed HDAC inhibitors target essential parasite epigenetic machinery, offering a powerful but complex frontier for next-generation antiparasitic therapy.
Read More Articles
Spatial Collapse: Pharmacologic Degradation of PDEδ to Disrupt Oncogenic KRAS Membrane Localization
PDEδ degradation disrupts KRAS membrane localization to collapse oncogenic signaling through spatial pharmacology rather than direct enzymatic inhibition.
Neumedics’ Integrated Innovation Model: Dr. Mark Nelson on Translating Drug Discovery into API Synthesis
Dr. Mark Nelson of Neumedics outlines how integrating medicinal chemistry with scalable API synthesis from the earliest design stages defines the next evolution of pharmaceutical development.
Zentalis Pharmaceuticals’ Clinical Strategy Architecture: Dr. Stalder on Data Foresight and Oncology Execution
Dr. Joseph Stalder of Zentalis Pharmaceuticals examines how predictive data integration and disciplined program governance are redefining the future of late-stage oncology development.
Exelixis Clinical Bioanalysis Leadership, Translational DMPK Craft, and the Kirkovsky Playbook
Senior Director Dr. Leo Kirkovsky brings a rare cross-modality perspective—spanning physical organic chemistry, clinical assay leadership, and ADC bioanalysis—to show how ADME mastery becomes the decision engine that turns complex drug systems into scalable oncology development programs.
Policy Ignition: How Institutional Experiments Become Durable Global Evidence for Pharmaceutical Access
Global pharmaceutical access improves when IP, payment, and real-world evidence systems are engineered as interoperable feedback loops rather than isolated reforms.







