
In recent years, the peptide drug discovery field has grown substantially across academia and the pharmaceutical industry. Over 60 peptide drugs have been FDA-approved, and over 150 peptides are in active development today, entering human clinical studies at a steady pace. Oncology and neurology are two therapeutic areas in particular, which are benefiting from peptide drug discovery.
Introduction
Peptides represent a unique class of biological compounds, many of which are intrinsic signaling molecules for a multitude of physiological functions. These compounds are short chains of amino acids, which are connected to each other by peptide bonds. Proteins are made up of multiple peptide subunits, and so are also known as polypeptides.
As therapeutic agents, peptides offer a number of advantages relative to small molecules including simpler design, ability to interact with underexplored targets, cheaper synthesis, decreased immunogenicity and enhanced tissue penetration.
Unfortunately, peptide therapeutics have faced a number of challenges in the past, which has slowed drug development and seen small molecule drugs take the lead. Short plasma half-life has been a particular issue, especially for peptide hormones – this arises due to the body’s desire to maintain homeostasis, so clears excessive levels of any peptides that arise.
Oral bioavailability has also been a difficult hurdle to overcome, due to the fact that digestive enzymes designed to break down the bonds of ingested proteins, are also effective at degrading the same bonds in peptides. As oral delivery is one of the most appealing forms of drug administration, in terms of patient compliance, peptide therapeutics were a less appealing option for indications which required chronic treatment.
Innovations in synthetic biology, have allowed for the modulation of pharmacokinetic properties of peptide therapeutics. Amino acid or backbone modification (and other changes) are a few ways that have shown to extend half-life or improve solubility.
Novel formulation strategies have also reduced the need for frequent injections and improved stability, and as a result, injection is viewed as an acceptable route of administration for certain indications, partly due to the development of longer-acting peptides.
Therapeutic applications
Cancer
Peptide drug conjugates (PDCs) are an emerging targeted therapeutic in oncology, that presents increased tumour penetration and selectivity. New approaches aim to address some of the previous limitations for the use of peptides as therapeutic agents, and demonstrate the great promise of these drugs for cancer. These drugs possess a similar construct to that of ADCs, and comprise three vital components: a homing peptide, a linker and a cytotoxic payload.
Tumour homing peptides are described as “cyclic or linear peptides of few amino acids having inherent property to recognize the tumor cells, which specifically bind to the receptors present on the tumor cells, tumor blood vessels or tumor lymphatic vessels.”
The mechanism of action for a PDC varies depending on several factors, including, the linker and homing peptide and is typically one of two scenarios:-
The first, is where the PDC will follow a similar process to that of an ADC. The binding of the PDC to the target causes internalisation after which, intracellular cleavage releases the cytotoxin. An alternative scenario occurs, when cleavage occurs outside the cell, followed by internalisation of the cytotoxin. Homing peptides can be cell penetrating or non-cell penetrating peptides, hence play an important role in this mechanism of action.
While the market of antibody drug-conjugates (ADCs) continues to grow at an exponential rate, the same cannot be said for PDCs. Overcoming some of the issues with poor pharmacokinetic properties of peptides and formulation has been slow, and only recently pharmaceutical companies have started to expand their pipelines to accommodate peptide therapeutics.
Inhibitory, or interference peptides (iPeps) have also emerged as a promising approach for the design of drug candidates in oncology. These peptides can target large surface areas, which enables them to achieve high selectivity as biologics, as well as effectively entering cells, and reaching intracellular targets as well as small molecules.
Relevant studies have demonstrated the potential of iPeps to inhibit central oncogenes, such as MYC, HOX, and HDM2/HDMX (in vitro and in vivo). However, it is key that iPep technology overcomes certain obstacles, like poor half-life in circulation, to maximise their therapeutic potential, before proceeding further to clinical studies.
177-Lu-dotatate is currently the only therapeutic PDC on the market, and is used to treat gastroenteropancreatic neuroendocrine tumours (GEP-NETs) – it was the first FDA approved PDC.
Multiple sclerosis
In recent years, peptide therapeutics has been a particular area of interest for multiple sclerosis (MS) – a disease of the central nervous system, in which the immune system attacks the insulating layer around the axon of neurons.
As of now, there is no cure for MS however, it is possible to treat the symptoms with a number of drugs – this is dependent on the specific symptoms and challenges the person has. For relapsing MS, patients are often prescribed a 5-day course of steroid tablets to be taken at home, or injections of steroids given in hospital for 3 to 5 days. While this treatment speeds up the recovery from the relapse, it doesn’t prevent further relapses, nor does it stop disease progression.
Recently, biotechnology company Apitope, has been developing therapeutic peptides to induce the suppression of the autoimmune responses toward self-antigens. According to an article, their latest phase II, a trial for the candidate ATX-MS-1467, has revealed promising data for the treatment of MS.
Apitope’s technology uses specific peptides, which induce an antigen-specific expansion of regulatory T cells – the cells can suppress the helper T cells, which produce the proinflammatory cytokines that are responsible for the pathology, in autoimmune diseases like MS.
In a recent press release, Dr Keith Martin, Chief Executive Officer of Apitope, commented: “We are delighted with these positive results that confirm both clinical findings in our Phase Ib trial as well as preclinical results showing significant decreases in MRI detected lesions and disability in a standard multiple sclerosis model. We will continue to progress the development of ATX-MS-1467 as a treatment for multiple sclerosis and are currently preparing for a Phase IIb placebo controlled study to demonstrate clinical efficacy.”
The announcement of a phase IIb placebo study is extremely encouraging for peptide therapeutics, which should provide further information on the effects after a longer treatment period. If the clinical study continues to yield promising results, this might introduce a much safer approach to MS treatment than stem cell transplantation, which has been associated with life-threatening complications.
It’s hoped that continued research efforts and advancements in technology will overcome the slow progression for peptide therapeutics to get into the clinic and address the challenges of pharmacokinetics and limited oral bioavailability.
Charlotte Di Salvo, Editor & Lead Medical Writer
PharmaFeatures
Subscribe
to get our
LATEST NEWS
Related Posts

Drug Discovery Biology
Proteolytic Rewriting: Engineering Controlled Absence of Pathogenic Protein Persistence
Targeted protein degradation transforms drug therapy by engineering the cellular machinery to erase, rather than merely inhibit, pathogenic proteins.

Drug Discovery Biology
Open Nucleotides: Grant-Driven Infrastructure for Equitable mRNA Vaccine Manufacturing
By developing accessible cap analogs and RNA raw materials, Hongene Biotech, guided by David Butler’s expertise in nucleotide chemistry and supported by the Gates Foundation, is reshaping the molecular infrastructure that underpins global mRNA vaccine equity.
Drug Discovery Biology
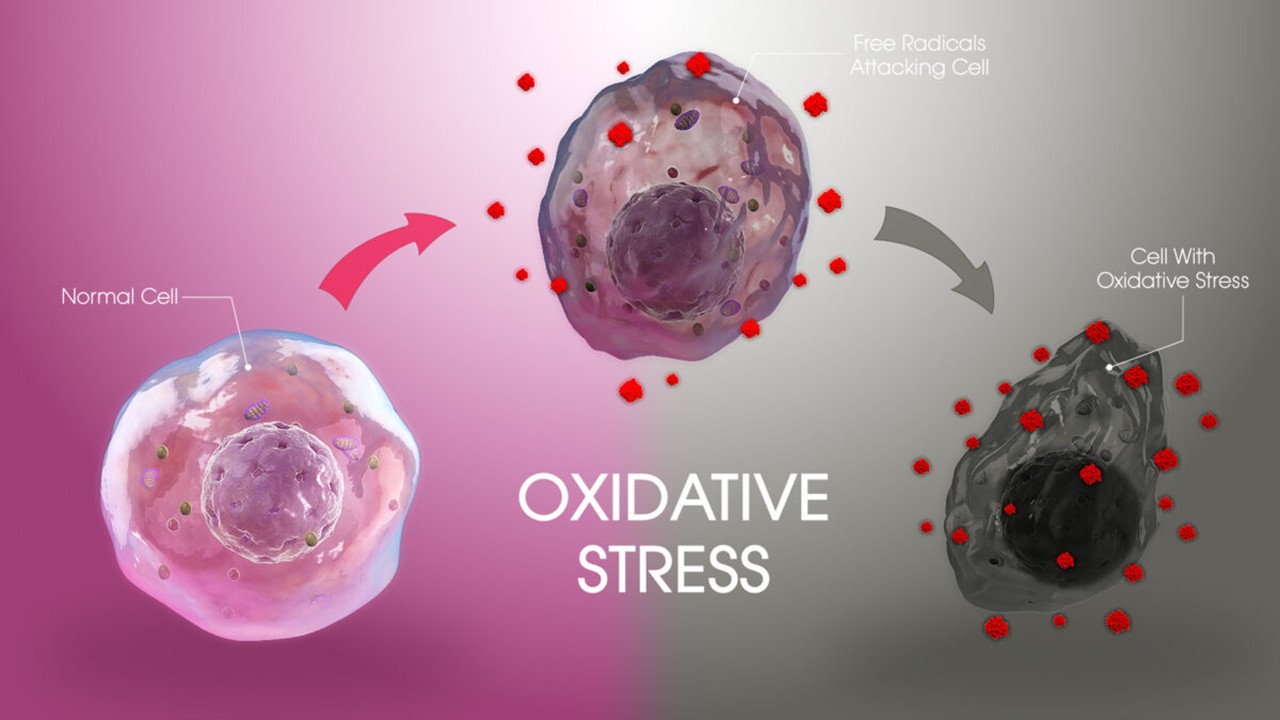
Redox Messengers: How Endogenous Gasotransmitters Rewire Vascular Biology to Resist Age-Driven Oxidative Stress
Gasotransmitters provide a biologically sophisticated means of counteracting age-related oxidative stress and preserving vascular resilience.
Drug Discovery Biology
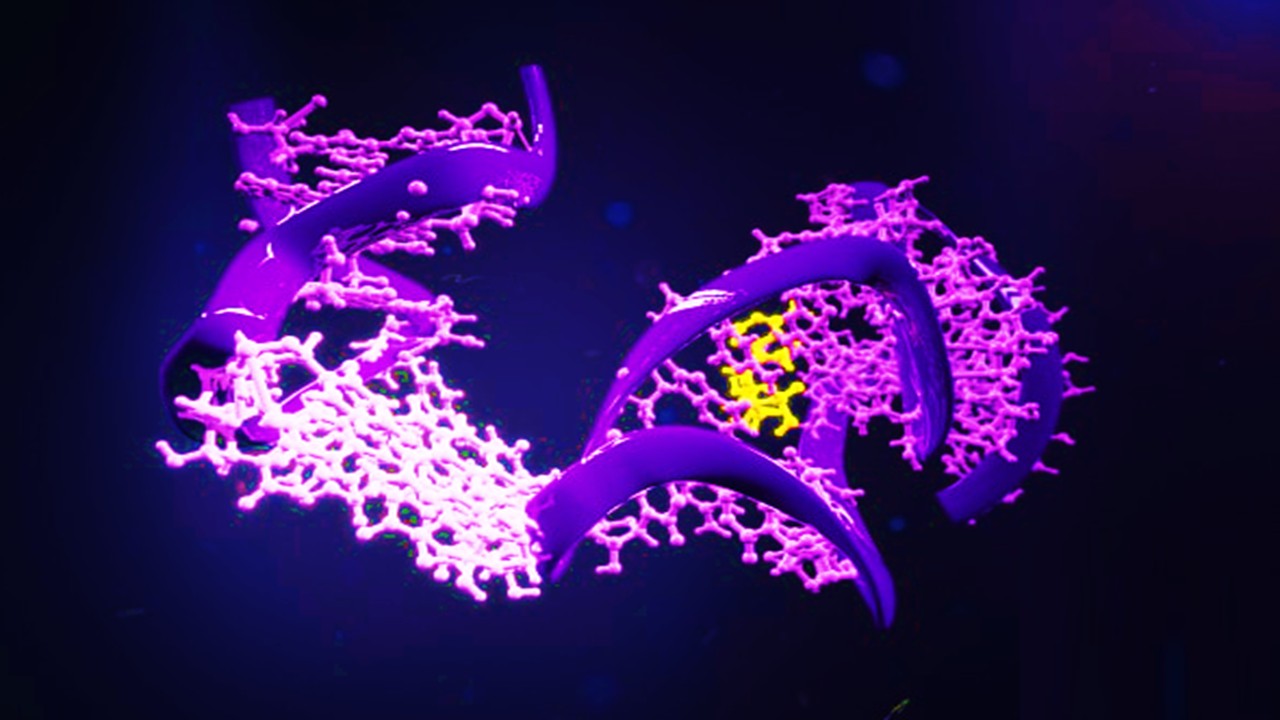
Aptamer Signal Dynamics: Engineering Nucleic Acid Recognition Systems for High-Fidelity, Multi-Modal Biosensing
Aptamers redefine biosensing by pairing programmable molecular recognition with versatile transduction strategies capable of detecting clinically relevant biomarkers with exceptional fidelity.
Read More Articles
Spatial Collapse: Pharmacologic Degradation of PDEδ to Disrupt Oncogenic KRAS Membrane Localization
PDEδ degradation disrupts KRAS membrane localization to collapse oncogenic signaling through spatial pharmacology rather than direct enzymatic inhibition.
Neumedics’ Integrated Innovation Model: Dr. Mark Nelson on Translating Drug Discovery into API Synthesis
Dr. Mark Nelson of Neumedics outlines how integrating medicinal chemistry with scalable API synthesis from the earliest design stages defines the next evolution of pharmaceutical development.
Zentalis Pharmaceuticals’ Clinical Strategy Architecture: Dr. Stalder on Data Foresight and Oncology Execution
Dr. Joseph Stalder of Zentalis Pharmaceuticals examines how predictive data integration and disciplined program governance are redefining the future of late-stage oncology development.
Exelixis Clinical Bioanalysis Leadership, Translational DMPK Craft, and the Kirkovsky Playbook
Senior Director Dr. Leo Kirkovsky brings a rare cross-modality perspective—spanning physical organic chemistry, clinical assay leadership, and ADC bioanalysis—to show how ADME mastery becomes the decision engine that turns complex drug systems into scalable oncology development programs.
Policy Ignition: How Institutional Experiments Become Durable Global Evidence for Pharmaceutical Access
Global pharmaceutical access improves when IP, payment, and real-world evidence systems are engineered as interoperable feedback loops rather than isolated reforms.
Sepsis Shadow: Machine-Learning Risk Mapping for Stroke Patients with Bloodstream Infection
Regularized models like LASSO can identify an interpretable risk signature for stroke patients with bloodstream infection, enabling targeted, physiology-aligned clinical management.







