With over 5% of the world population (when considering only confirmed cases) having had COVID-19, the disease caused by infection with SARS-CoV-2, our need to understand the full impact of consequences from infection cannot be understated. It is well established that, in addition to acute COVID-19 syndrome, chronic sequelae can often follow – what we call long COVID. We have already explored the impact of coronavirus on the central nervous system in a different article. Today, we will be discussing the effects that infection has on the cardiovascular and circulatory systems.
Cellular Entry
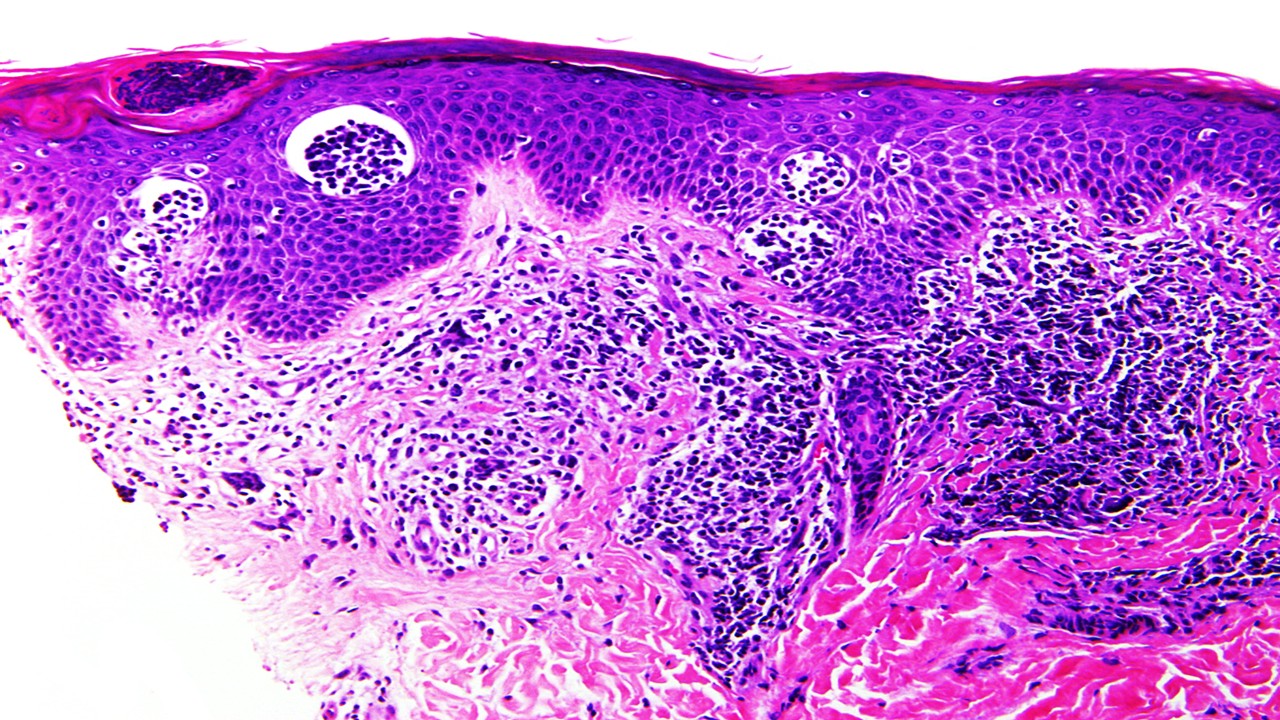
It is now understood that the most important cellular receptor for SARS-CoV-2 is the Angiotensin-converting enzyme 2 (ACE2) receptor, which facilitates entry of the virus within the cell. Early in the pandemic, the presence of this receptor was identified in a wide breadth of organs and tissues – including the lungs, brain, heart, epithelial cells, kidneys and elsewhere. The ability of the virus to enter organs beyond the lungs is not questioned – the presence of the virus in the human heart was already confirmed in autopsies of COVID-19 patients early in the pandemic.
Studies specifically focusing on studying cardiovascular ACE2 receptors noted an increased presence of ACE2 in the hearts of patients with comorbidities, such as aortic stenosis, a history of heart failure, obesity, diabetes. Obese and diabetic patients also showed increased cardiac expression of other proteins related to viral entry, such as Transmembrane serine protease 2 (TMPRSS2), metalloproteases ADAM10 and ADAM17. Additionally, medications often taken to lower blood pressure or treat associated cardiovascular conditions have been found to increase the expression of ACE2 in the heart, lungs, and other parts of the body.
The above findings suggest a complex relationship between the virus and cardiovascular disease. In the early days of the pandemic, it was obvious that reduced cardiovascular and pulmonary function was a risk factor for disease severity with the coronavirus, but the reverse – COVID-19 increasing the long-term risk for heart disease – is also recognized as a very real possibility now.
Chronic Symptoms
A new study published in Nature this February examined the long-term increases in risk for cardiovascular incidents subsequent to acute COVID-19, with worrying findings. Survivors of the disease demonstrated significantly higher risk for a host of conditions, such as cerebrovascular disorders, dysrhythmias, inflammatory heart disease, ischemic heart disease, thrombotic disorders and other heart conditions 12 months after recovery.
The excess burden of these conditions was starkly higher in patients who had to be admitted to a hospital during the acute phase of the infection – and even more so in those admitted to Intensive Care Units (ICU), suggesting a strong correlation between disease severity and long-term symptoms. This is congruent with findings from other studies which exhibited higher risk for more survivors who required more advanced care during the main COVID-19 infection across a range of conditions – including pulmonary, cardiac, circulatory, mental and nervous system symptoms. However, the risk increase remains significant even for patients who did not require hospitalization.
Mechanisms of Action
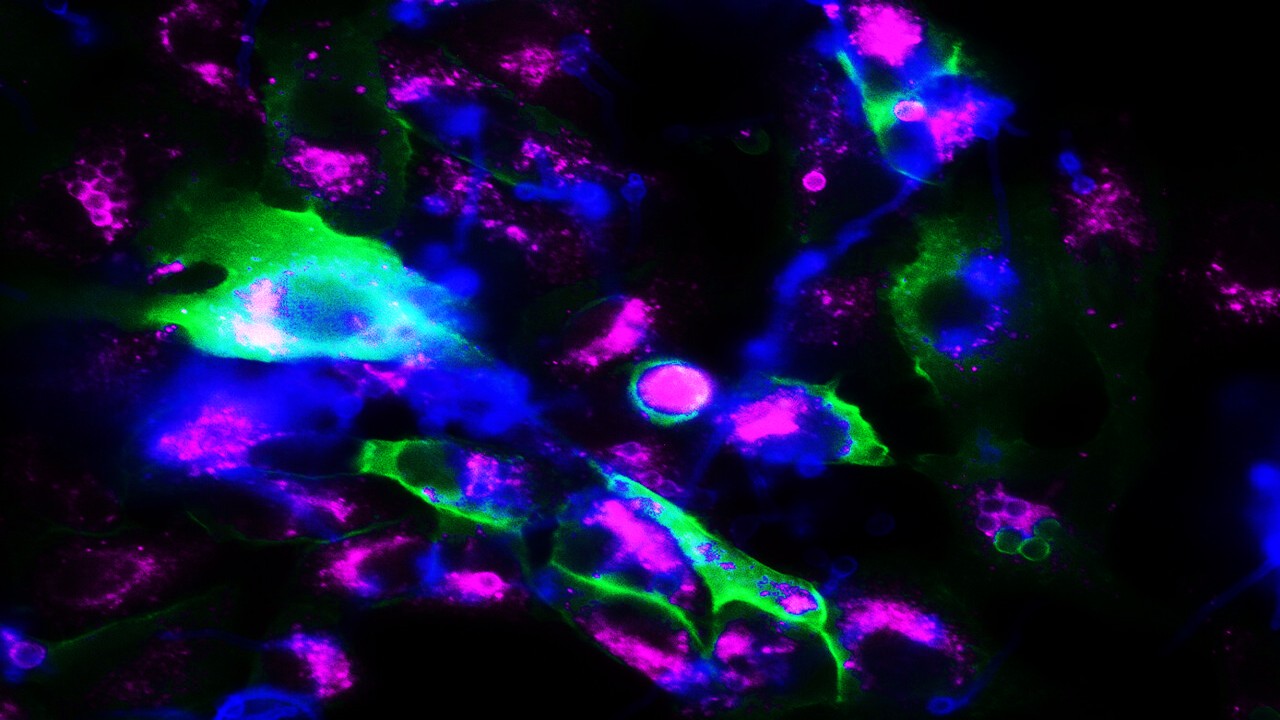
These studies have indicated robust interactions to demonstrate the contribution of excess burden on heart disease caused by COVID-19. We yet lack a definitive understanding of how this growth in mortality comes about however – though there is a plethora of putative mechanisms that are being investigated. These include direct viral damage – given the presence of ACE2 receptors. Inflammation caused by the immune system in response to the virus, including the prothrombotic cascade, is another plausible mechanism that could explain the extent of the damage seen beyond the pulmonary system, through the formation of microthrombs, neutrophils being trapped in the extracellular matrix and other phenomena.
Immune system dysregulation may also be a possible cause – it is known that overactivation of the immune response can be a leading cause for the more severe clinical presentations of COVID-19. This is particularly so in the form of a cytokine storm. Severe infection may result in the generation of autoantibodies, which can persist and lead to complications for the duration of their existence within the body. Realistically, a diverse combination of contributing factors will be involved – as that would explain the great diversity of clinical manifestations of long COVID, with a diverse array of symptoms in different tissues and organs, across different patients.
Future Outlooks
The investigations into the increased burden of cardiopathies caused by COVID-19 highlight the need for further study into the exact cellular and molecular mechanisms by which long COVID can impact the body. However, the technologies we pioneered during the pandemic are already seeing application in improving other therapeutic areas – mRNA-based therapeutics, in particular, have been experiencing a resurgence on the back of the highly successful mRNA COVID-19 vaccines. In the area of heart health, an AstraZeneca-Moderna partnership has been aiming to facilitate the regeneration of heart tissue following cardiac incidents, using mRNA treatments that can stimulate the growth of epithelial cells – billions of which are lost during a heart attack.
Another important insight from the investigations surrounding long COVID-19 is the significance of going beyond the measuring of deaths for the pandemic. It is critical to be more inclusive, and consider the cost of the disease through other measures; as our awareness of the chronic implications of COVID-19 increases, so does the need to quantify the possible impact that we will be facing from them. DALYs, Disability Adjusted Life Years, measure the number of years lived with disability or lost because of premature death, and are effective in characterizing the impact of a disease. Although they are uncommon for health infrastructures in higher income countries, unlike low and middle income countries that have used them to great effect in recent times, this is expected to change.
Furthermore, we must improve the care we provide to COVID-19 survivors, through the use of innovative biomarkers and monitoring technologies – such as cardiac Magnetic Resonance Imaging to lower the impact of cardiovascular disease. As we move past the acute stage of the pandemic – particularly after the Omicron wave, it is becoming increasingly clear that the consequences of the coronavirus will remain with us far in the future. Though we are only just beginning to address these new problems, the pharmaceutical industry and the world at large have shown great resilience and innovation in countering novel threats: we must continue to do so.
Nick Zoukas, Former Editor, PharmaFEATURES
Subscribe
to get our
LATEST NEWS
Related Posts

Infectious Diseases & Vaccinology
Enduring Blockade: Five-Year Functional Antibody Persistence Against Emerging GII.4 and GII.17 Noroviruses
Natural infection with dominant GII noroviruses elicits long-lived functional antibodies, redefining immune durability in viral gastroenteritis.
Infectious Diseases & Vaccinology
Resistant Mycosis: Reimagining Antifungal Therapy Through Mechanistic Innovation and Molecular Disruption
Emerging antifungal strategies are redefining treatment by targeting fungal physiology through diversified, mechanism-driven approaches that overcome entrenched drug resistance.
Infectious Diseases & Vaccinology
Fungal Refractory States: Deciphering Pathobiology and Therapeutic Weaknesses in the Era of Rising Antifungal Resistance
Rising antifungal resistance reflects a multidimensional biological challenge that demands mechanistically innovative, host-integrated therapeutic strategies.

Infectious Diseases & Vaccinology
Epigenetic Parasite Vulnerabilities: Repurposing Histone Deacetylase Inhibitors for Complex Multispecies Therapeutics
Repurposed HDAC inhibitors target essential parasite epigenetic machinery, offering a powerful but complex frontier for next-generation antiparasitic therapy.
Read More Articles
Spatial Collapse: Pharmacologic Degradation of PDEδ to Disrupt Oncogenic KRAS Membrane Localization
PDEδ degradation disrupts KRAS membrane localization to collapse oncogenic signaling through spatial pharmacology rather than direct enzymatic inhibition.
Neumedics’ Integrated Innovation Model: Dr. Mark Nelson on Translating Drug Discovery into API Synthesis
Dr. Mark Nelson of Neumedics outlines how integrating medicinal chemistry with scalable API synthesis from the earliest design stages defines the next evolution of pharmaceutical development.
Zentalis Pharmaceuticals’ Clinical Strategy Architecture: Dr. Stalder on Data Foresight and Oncology Execution
Dr. Joseph Stalder of Zentalis Pharmaceuticals examines how predictive data integration and disciplined program governance are redefining the future of late-stage oncology development.
Exelixis Clinical Bioanalysis Leadership, Translational DMPK Craft, and the Kirkovsky Playbook
Senior Director Dr. Leo Kirkovsky brings a rare cross-modality perspective—spanning physical organic chemistry, clinical assay leadership, and ADC bioanalysis—to show how ADME mastery becomes the decision engine that turns complex drug systems into scalable oncology development programs.
Policy Ignition: How Institutional Experiments Become Durable Global Evidence for Pharmaceutical Access
Global pharmaceutical access improves when IP, payment, and real-world evidence systems are engineered as interoperable feedback loops rather than isolated reforms.







