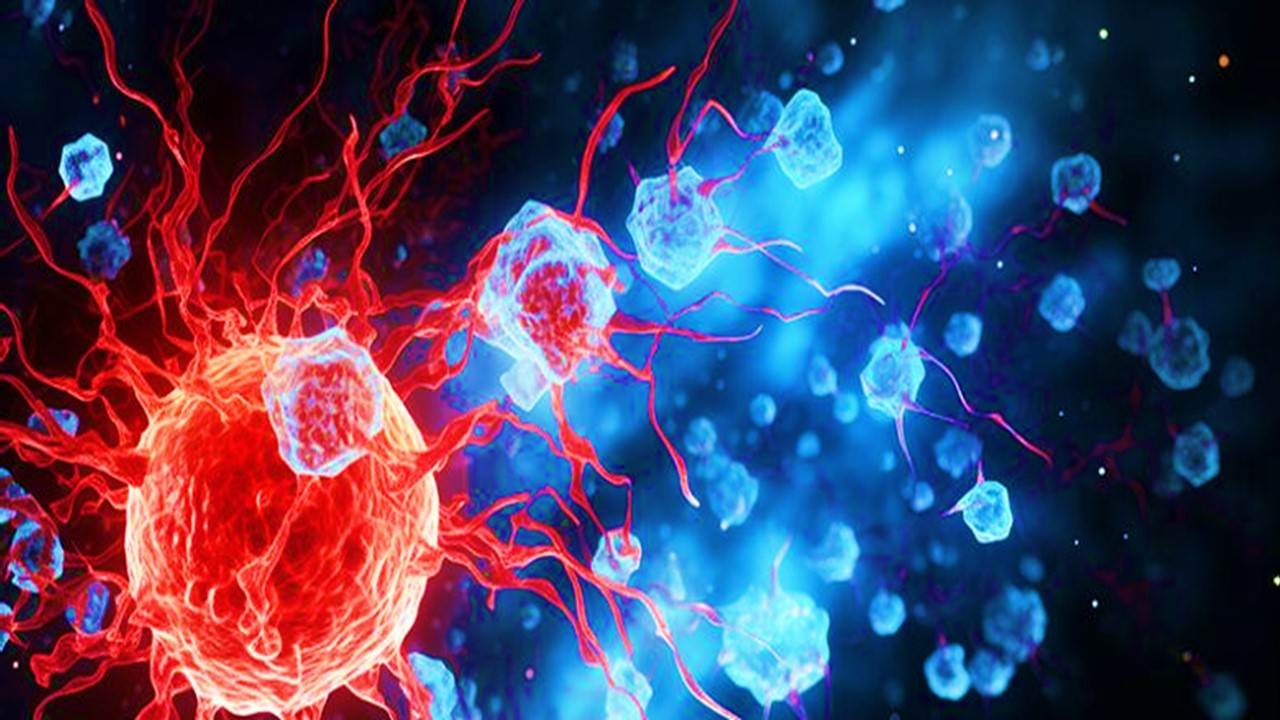
The body’s protection against infectious pathogens is the immune system. By recognizing and neutralizing substances that are perceived as nonself, it defends the host. Practically every organ, tissue, and cell in the body is impacted by the full spectrum of immunological reactions. The generation of antibodies (Ab), allergies, inflammation, phagocytosis, cytotoxicity, transplant and tumor rejection are some examples of immune responses, as are the numerous signals that control these reactions. The cells that make up the human immune system can be used to define it at its most fundamental level. A group of specialized cells regulates every component of the immune system, whether it is innate and nonspecific or adaptive and particular. Consequently, the immune system’s cells serve as the starting point for this examination of some of the essential concepts in immunology.
Deriving Immunity from Pluripotency
Pluripotent stem cells inside the bone marrow are the source of all immune cells. They are cells that, given the proper stimuli, can develop into any other form of cell. Unique cellular types with distinct roles in the immune system are created through a variety of processes of differentiation that extend beyond the stem cell. Two intermediate types of stem cells as well as a branch point are produced during the initial stage of differentiation. Myeloid (myeloid lineage) and lymphoid cells make up these cells (lymphoid lineage). Further branching results from continuing the lineage. Myeloid cells undergo differentiation to form erythrocytes, platelets (thrombocytes), monocytes, and granulocytes. The lymphoid cell undergoes differentiation to produce B cells and T cells, which are essential for adaptive immunity. Many colony-stimulating factors, stem cell factors, and interleukins control the switching system for each pathway and cell type. They regulate the cell’s ability to divide, differentiate, and mature.
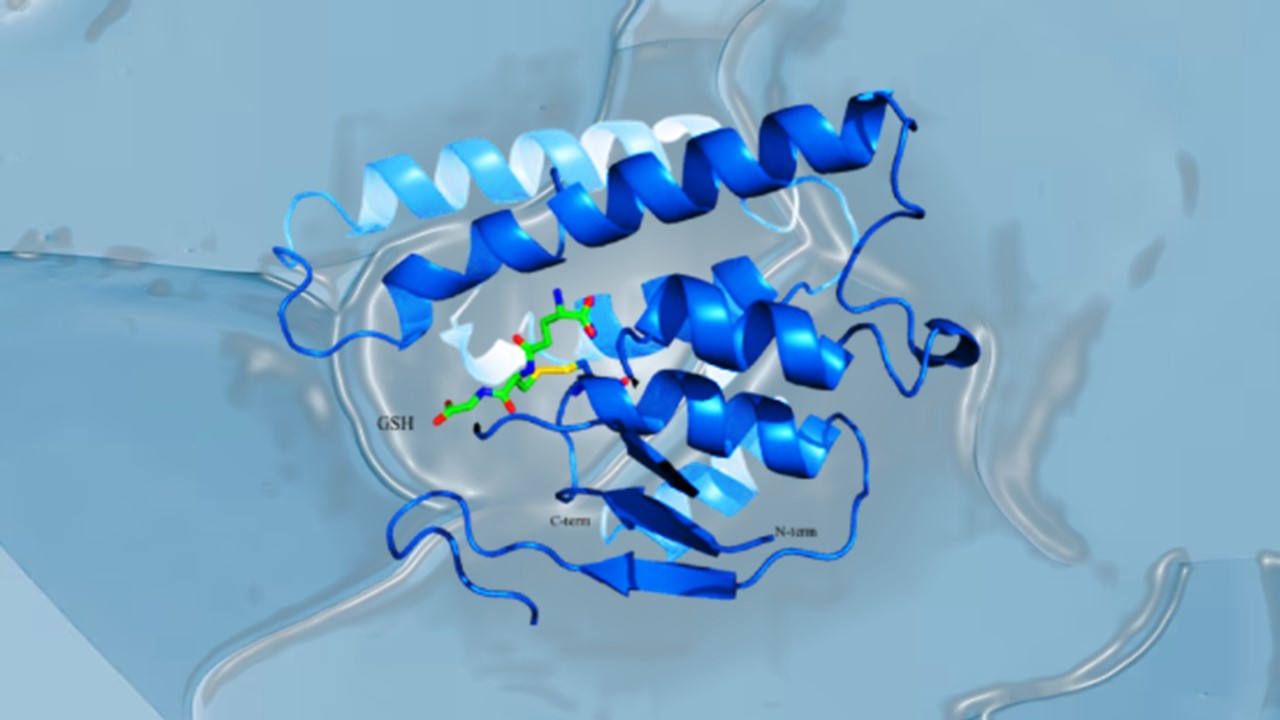
Recognizing Self versus Nonself
Recognition of what is self and what is not self is necessary for the development of the majority of immune responses. This choice must be made with clarity and in a broad sense. Specialized surface markers are expressed on human cells to facilitate this recognition. Surface proteins make up the main class of markers in this recognition. Major Histocompatibility Complex (MHC) or major histocompatibility antigens are the terms used to describe these. Class I and class II MHC proteins are found on the cell surfaces. Both classes are extremely polymorphic and hence highly individualized. Almost all nucleated human cell types include class I MHCs, whereas class II MHC molecules are exclusively found on B lymphocytes and macrophages. Class I MHCs are antigens that are acknowledged by cytotoxic T lymphocytes and natural killer cells. Cytotoxic target cells are alerted when a class I MHC coexpresses with viral antigens on virus-infected cells. When a cooperative immunological state exists between immunocompetent cells, such as between an antigen-presenting cell (APC) and a T-helper cell during the stimulation of Ab production, Class II MHC molecules serve as indicators.
Granulocytes
Under microscopy, dense intracytoplasmic granules can be seen in granulocytes. The granules include digestive enzymes and proinflammatory cytokines that kill invasive infections, regulate the rate and direction of chemotactic cell migration, and widen blood arteries at the infected location. A sufficient amount of granulocytes and inflammatory mediators are delivered to the infection site thanks to the increased blood flow. Granulocytic cells are a family, and each member has a unique purpose. A microscopic inspection reveals that some granulocytes are multinuclear and others are mononuclear. Granulocytes can be categorized using the nuclear region’s structure and staining behavior.
Neutrophils
The main innate defense against harmful microorganisms is provided by neutrophils. They account for the majority (50–75%) of the blood’s leukocyte percentage. Neutrophils have multilobed nuclei under a microscope. Chemotaxis is the process by which they move toward an infection site in response to chemical motility cues, such as complement mediators released from infected or inflamed tissues. They identify, cling to, and phagocytoze invasive bacteria there.
Phagocytes
The interaction and adherence of an invasive cell with a phagocyte cellular membranes starts the phagocytic process. The phagocytic cell produces pseudopodia that envelop the adherent pathogen as a result of attachment. The phagocyte cellular membrane really surrounds the microorganism as this process continues. When the membrane has completely engulfed the particle, it is resealed, and the particle is contained inside an intracellular vacuolar body known as a phagosome. The phagosome then fuses with lysosomes in the cytoplasm to create phagolysosomes. The encapsulated pathogen is killed by the antibacterial substances in the phagosomes and lysosomes, which also enzymatically split the pathogen’s remnants into smaller fragments.
Eosinophils
Granulocytes called eosinophils can act as phagocytes but do so considerably less effectively than neutrophils. They make up 2% to 4% of the blood’s leukocytes. Their name is a result of the intracellular granules’ strong eosin staining reactivity. It makes sense that eosinophil granules, which contain inflammatory mediators like histamine and leukotrienes, are linked to the allergic response. The behavior of eosinophils in specific disease situations provides hints about their functions. Despite the fact that eosinophil counts are elevated above normal in the tissues in a wide range of disorders, they are largely known for their diagnostic value in parasite infections and allergies. Eosinophils are extremely important due to their distinctive mechanism of action. Eosinophils, unlike neutrophils, do not need to phagocytose a parasite in order to destroy it. It’s true that certain parasites are too big to be phagocytosed. Large parasites can be physically encircled by eosinophils, which surround the invader with a cell coat. Granules of eosinophils emit oxidative chemicals that can kill even big, multicellular parasites. Thus, a technique to eliminate big parasites persists even when phagocytosis fails..
Mast Cells and Basophils
The inflammatory mediators frequently linked to allergy are also released by mast cells and basophils. On the skin, lungs, and nasal mucosa, mast cells are particularly common. The autacoid histamine is particularly found in their granules. Basophils, which make up only 0.2% of the blood’s leukocyte component, are also known to contain histamine granules, however they are often seen circulating in blood rather than isolated in connective tissue. High-affinity immunoglobulin E (IgE) receptors are present on basophils and mast cells alike. IgE becomes cross-linked and the cell membrane becomes distorted when antigen molecules interact with IgE receptors on the cell surface. The mast cell degranulates as a result of the deformation, releasing mediators of the allergic reaction. IgE has been referred to in allergy literature as “reagin” due to its link to hypersensitivity. IgE levels are increased in rheumatoid arthritis, systemic lupus erythematosus, and allergy as diagnostic indicators. Drugs like cromolyn sodium stop mast cell degranulation, which stops the allergic reaction. It is for this very reason that cromolyn is indicated in asthma patients.
Macrophages and Monocytes
The mononuclear cells that can phagocytose are macrophages and monocytes. They have the ability to phagocytose, but they also biologically synthesize and release soluble components that control the acquired immune response (complement, monokines). Monocytes have a half-life of roughly 10 hours in the bloodstream, during which time they travel into tissues and undergo macrophage differentiation. A terminally differentiated monocyte is referred to as the macrophage. Macrophages grow in the tissues to establish specialized roles, which gives them a genuine anatomical distribution. Tissues such the liver, lungs, spleen, gastrointestinal (GI) tract, lymph nodes, and brain contain specific macrophages. These particular macrophages are known as histiocytes (a general term) or by other more specific names (microglial cells in the brain, alveolar macrophages or dust cells in lung, Kupffer cells in liver, dendritic cells in spleen, peritoneal macrophages in peritoneum, and Langerhans cells in skin).
The reticuloendothelial system refers to the complete macrophage network. Throughout the tissues, other macrophages are present in free form and perform other non-specific tasks. Although they have a far wider spectrum than neutrophils, macrophages kill more slowly. More than 100 soluble inflammatory chemicals are thought to be generated by macrophages. These compounds are responsible for the extensive control, modulation, stimulation, and inhibition of the immune response by macrophages.
Macrophages serve as APCs, which is a fairly specialized task. The preprocessing of antigens, the amplification of antigenic determinant units, and the presentation of these determinant structures to the immune system’s regulatory cells are all carried out by APCs. An organism or particle is internally digested by APCs into tiny pieces that are still recognizably antigen. The molecules of the major histocompatibility complex 2 (MHC-II) are coupled with the fragments. These complexes determine whether cells are self or nonself and confirm that the cells being processed are not self. Moreover, MHCs control how an antigenic determinant binds to immune-reactive cells. As soon as the antigen-MHC-II complex is formed, it is transcytosed to the macrophage’s cell surface, where B lymphocytes and T-helper cells are able to identify the antigen through the B surface Ab and T-cell receptors. As a result of this step’s modification of B-cell differentiation, the immune system receives specificity and memory information from the determinant. T-helper cells have a regulatory effect on B cells, encouraging them to develop into plasma cells that generate Ab. The process can be sped up or slowed down as needed by the T-helper cells. So, unlike granulocytes, which only perform damaging tasks, monocytes and macrophages control and direct the immune response.
The Lymphoid Cell Line: B and T Cells
B lymphocytes and T lymphocytes are the two types of lymphocytes that are produced from the lymphoid cell line. The percentage of these cells in blood leukocytes ranges from 20% to 45%. Although B and T cells are tiny, just a little bigger than erythrocytes, they may be distinguished under a microscope by their enormous nuclei, which take up the majority of the cytoplasmic space. The big nuclei allow the T and B cells to biosynthesize enormous amounts of protein required for performing their immunological tasks. Cell-mediated immunity (CMI) is mediated by T lymphocytes, whereas B lymphocytes develop into plasma cells that produce antibodies (Abs). B cells produce antibodies that attach to antigens on their surfaces. Major Histocompatibility Complex 1 (MHC-I) and 2 (MHC-II) complexed with antigenic peptide fragments are recognized by specific T-cell receptors expressed on the surfaces of T cells.
Engr. Dex Marco Tiu Guibelondo, BS Pharm, RPh, BS CpE
Editor-in-Chief, PharmaFEATURES