The Kinome: A Cellular Orchestra in Health and Disease
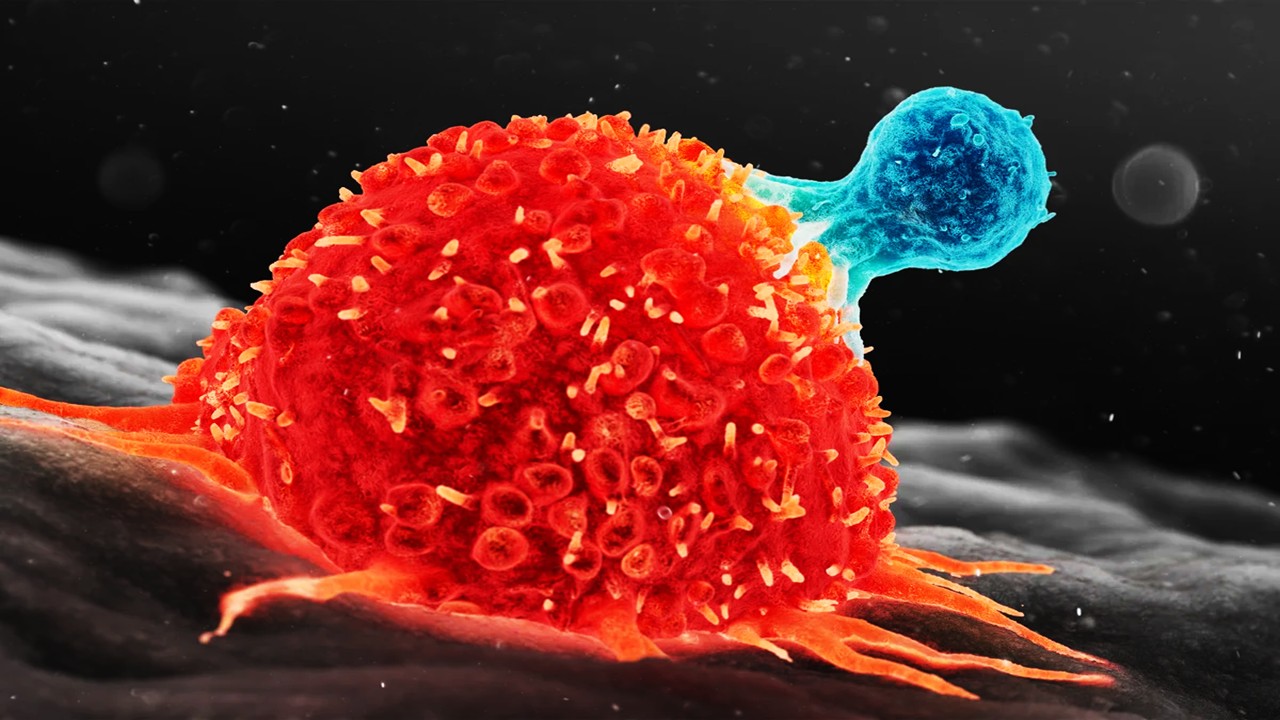
Protein kinases act as conductors of cellular communication, orchestrating signals that regulate growth, survival, and death. Their dysregulation is a hallmark of cancer, where mutations or overexpression transform kinases into drivers of uncontrolled proliferation. Over 70 kinase inhibitors are clinically approved, targeting oncogenic players like EGFR and BRAF, yet their efficacy is often hindered by off-target effects and resistance. The kinome’s complexity—spanning over 500 kinases with conserved ATP-binding pockets—demands a holistic view of inhibitor interactions. Understanding how drugs modulate the entire kinome, rather than isolated targets, could revolutionize precision oncology.
Traditional drug development focuses on singular kinase targets, but cancer cells exploit kinome-wide network plasticity to evade treatment. This adaptability underscores the need to map inhibitor effects across the entire kinome. High-throughput assays like Kinobeads and KINOMEscan capture these interactions, profiling hundreds of kinases per compound. Kinobeads analyze native kinases in cell lysates, preserving post-translational modifications, while KINOMEscan screens recombinant kinases for binding affinity. Together, they create a comprehensive atlas of inhibitor-kinome engagement.
Understudied kinases, termed the “dark kinome,” represent uncharted therapeutic opportunities or hidden resistance mechanisms. These kinases lack functional annotation or chemical probes, limiting their exploration. Integrating multi-omic data—gene expression, mutations, and proteomics—contextualizes their roles within cellular ecosystems. Machine learning models trained on this data predict how kinome-wide inhibition states correlate with drug sensitivity. This approach shifts the paradigm from target-centric to network-centric drug design.
The kinome’s dual role as driver and bystander complicates therapeutic targeting. While some kinases directly fuel tumorigenesis, others modulate survival pathways indirectly. Predictive models must account for these network effects to avoid oversimplification. By decoding kinome inhibition states, researchers can identify synergistic targets and repurpose existing drugs. This systems-level understanding bridges molecular profiling to clinical outcomes.
Cancer’s reliance on kinome plasticity necessitates tools that capture its dynamic nature. Static genomic snapshots fail to reflect real-time kinase activity, whereas kinome profiling provides actionable insights. Integrating these data with AI unlocks predictive power, guiding personalized therapy and overcoming resistance.
Mapping the Kinome: Integrating High-Throughput Profiling Data
Kinobeads and KINOMEscan offer complementary views of inhibitor-kinome interactions. Kinobeads use mass spectrometry to quantify kinase engagement in native cellular environments, preserving physiological contexts like protein complexes and post-translational modifications. KINOMEscan employs recombinant kinases to measure binding affinities in vitro, enabling rapid profiling of hundreds of compounds. Merging these datasets creates a unified resource spanning clinical and experimental inhibitors.
Data integration required meticulous normalization to reconcile assay-specific metrics. Kinobeads’ relative intensity values and KINOMEscan’s percent control measurements were harmonized, imputing missing data to reflect baseline activity. The resulting dataset covers ~1,000 inhibitors and ~800 kinases, including understudied targets. UMAP dimensionality reduction visualized inhibitor clusters, revealing shared kinome inhibition patterns across compounds.
Assay differences posed challenges: recombinant kinases lack native context, while cell lysates may miss in vivo dynamics. However, strong correlations between overlapping kinases validated integration feasibility. Inhibitors with consistent profiles across assays demonstrated higher predictive accuracy, underscoring the value of cross-validation.
This integrated kinome atlas captures both breadth and depth, encompassing FDA-approved drugs and tool compounds. It serves as a foundation for predictive modeling, linking inhibitor profiles to phenotypic responses. The resource is publicly accessible, empowering researchers to explore understudied kinases and repurpose existing therapies.
By bridging methodological gaps, this work highlights the kinome’s complexity and the need for multi-assay approaches. Future profiling efforts must prioritize underrepresented kinases to illuminate the dark kinome.
Machine Learning Models: Decoding Kinome-Phenotype Relationships
Predictive models were trained on kinome inhibition states and baseline transcriptomic data from cancer cell lines. LASSO regression, random forests, and XGBoost algorithms ranked features by their correlation with drug sensitivity. XGBoost outperformed others, achieving robust prediction accuracy by integrating kinase engagement and gene expression.
Shapley value analysis revealed kinases like FLT3 and understudied PIP4K2C as top predictors. FLT3, though associated with leukemia, influenced viability in lung cancer models, suggesting off-target effects. PIP4K2C, a lipid kinase, emerged unexpectedly, implicating metabolic pathways in drug response. Baseline gene expression provided cellular context, fine-tuning predictions to lineage-specific biology.
The model prioritized kinase inhibition states over transcriptomic data, emphasizing their direct mechanistic link to phenotype. However, gene expression enriched predictions for heterogeneous cell lines, capturing adaptive resistance mechanisms. This dual-input approach balances broad kinome effects with cell-specific vulnerabilities.
Understudied kinases ranked highly, validating their potential as therapeutic targets. For example, CSNK2A2, a casein kinase, correlated with poor prognosis across cancers. These findings challenge the conventional focus on well-characterized kinases, advocating for exploratory studies.
The model’s success lies in its ability to generalize across cancer types. By decoding kinome-wide patterns, it identifies actionable targets and predicts drug efficacy without prior mechanistic knowledge.
Validating Predictions: From Breast Cancer to Patient-Derived Models
Predictions were tested in HER2-positive (BT-474, SKBR3) and triple-negative (HCC1806, SUM159) breast cancer lines. Model-derived AUC/IC50 values aligned with experimental results, except in SKBR3, where HER2-independent survival pathways may drive resistance. Kinobeads-profiled inhibitors showed higher accuracy, reflecting native kinase interactions.
FLT3 inhibitors, though designed for leukemia, exhibited efficacy in lung cancer models, highlighting repurposing potential. Discrepancies in SKBR3 underscore the need to integrate microenvironmental factors, such as stromal interactions, into future models.
Patient-derived pancreatic cancer (PDAC) cell lines further validated the model. Predictions in stromal cells (R ~0.5) outperformed tumor lines (R ~0.3), reflecting transcriptional heterogeneity. KINOMEscan-profiled inhibitors showed lower accuracy due to limited training data, emphasizing the need for expanded datasets.
These validations confirm the model’s utility in prioritizing compounds for preclinical testing. Stromal models, with less genomic noise, better reflect kinome-driven phenotypes, guiding biomarker discovery.
Challenges in PDAC highlight the importance of diverse training data. Incorporating rare cancers and microenvironmental cues will enhance clinical relevance.
The Dark Kinome: Hidden Players in Drug Response
Understudied kinases like PIP4K2C and CSNK2A2 emerged as critical predictors, despite limited prior research. PIP4K2C modulates phosphoinositide metabolism, potentially influencing membrane trafficking in cancer cells. CSNK2A2 regulates Wnt signaling, a pathway central to stemness and resistance.
Off-target kinase interactors, including heat shock proteins, ranked highly in Shapley analysis. These findings implicate proteostasis in drug response, advocating for chemical proteomics to map non-kinase targets. Dark kinases may mediate adaptive resistance, offering novel therapeutic avenues.
The model’s ability to highlight these targets accelerates hypothesis generation. Functional studies are needed to elucidate their roles and validate their therapeutic potential.
This focus on understudied kinases challenges the bias toward well-characterized targets. Collaborative efforts must prioritize tool compound development for the dark kinome.
By illuminating these hidden players, the model bridges computational predictions and experimental oncology, fostering innovation.
Challenges and Limitations: Navigating Assay Heterogeneity
Assay-specific biases complicate data integration. Kinobeads capture native kinase complexes but lack throughput, while KINOMEscan offers scalability at the cost of physiological context. Discrepancies in overlapping kinases highlight the need for orthogonal validation.
Patient-derived models introduced transcriptional heterogeneity, reducing prediction accuracy. Stromal interactions and tumor microenvironment cues were absent in vitro, limiting clinical translatability. Future models must incorporate spatial omics and co-culture systems.
The reliance on single-dose profiling overlooks dynamic kinome adaptation. Time-resolved assays could capture compensatory signaling, improving prediction robustness.
Limited training data for KINOMEscan inhibitors constrained model performance. Expanding cell line screens will enhance generalizability.
These challenges underscore the importance of iterative model refinement. Addressing assay and biological complexity will unlock the kinome’s full predictive potential.
Future Directions: Toward Personalized Kinome-Targeted Therapies
The next frontier involves predicting synergistic inhibitor combinations to preempt resistance. Models analyzing dual kinome states could identify drug pairs that disrupt compensatory pathways.
Integrating CRISPR screens and proteomics will enrich predictions, linking genetic dependencies to kinase activity. Clinical trials could stratify patients by kinome states, enabling precision oncology.
Chemical proteomics platforms like thermal shift assays could expand kinome coverage, profiling non-ATP-binding kinases. Open-source datasets and collaborative consortia will democratize access to kinome profiling.
Dark kinase-focused drug discovery campaigns are urgently needed. Partnerships between academia and industry can accelerate probe development, transforming predictions into therapies.
Ultimately, AI-driven kinome profiling promises to democratize cancer treatment, turning molecular insights into actionable strategies for patients worldwide.
Study DOI: https://doi.org/10.7717/peerj.16342
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Subscribe
to get our
LATEST NEWS
Related Posts

Bioinformatics & Multiomics
Agentic Bioinformatics: How Autonomous AI Agents Compress Biomedical Discovery Cycles
Agentic bioinformatics treats biomedical discovery as a closed-loop system where specialized AI agents continuously translate intent into computation, computation into evidence, and evidence into the next experiment.

Bioinformatics & Multiomics
Proteomic Signatures: Molecular Discrimination of Hyperinflammatory States Through Serum Proteome Architecture
Serum proteomics exposes how sepsis and hemophagocytic syndromes diverge at the level of immune regulation and proteostasis, enabling precise molecular discrimination.

Bioinformatics & Multiomics
Residual Signals: Transcriptomic Surveillance and Multi-Domain Gene-Signature Mapping for Early Breast Cancer MRD Detection
MRD detection in breast cancer focuses on uncovering functional transcriptomic and microenvironmental signals that reveal persistent tumor activity invisible to traditional genomic approaches.
Read More Articles
Spatial Collapse: Pharmacologic Degradation of PDEδ to Disrupt Oncogenic KRAS Membrane Localization
PDEδ degradation disrupts KRAS membrane localization to collapse oncogenic signaling through spatial pharmacology rather than direct enzymatic inhibition.
Neumedics’ Integrated Innovation Model: Dr. Mark Nelson on Translating Drug Discovery into API Synthesis
Dr. Mark Nelson of Neumedics outlines how integrating medicinal chemistry with scalable API synthesis from the earliest design stages defines the next evolution of pharmaceutical development.
Zentalis Pharmaceuticals’ Clinical Strategy Architecture: Dr. Stalder on Data Foresight and Oncology Execution
Dr. Joseph Stalder of Zentalis Pharmaceuticals examines how predictive data integration and disciplined program governance are redefining the future of late-stage oncology development.
Exelixis Clinical Bioanalysis Leadership, Translational DMPK Craft, and the Kirkovsky Playbook
Senior Director Dr. Leo Kirkovsky brings a rare cross-modality perspective—spanning physical organic chemistry, clinical assay leadership, and ADC bioanalysis—to show how ADME mastery becomes the decision engine that turns complex drug systems into scalable oncology development programs.
Policy Ignition: How Institutional Experiments Become Durable Global Evidence for Pharmaceutical Access
Global pharmaceutical access improves when IP, payment, and real-world evidence systems are engineered as interoperable feedback loops rather than isolated reforms.