The Centers for Disease Control and Prevention (CDC) has recently taken the lead in the fight against a potentially fatal fungal meningitis outbreak that has been connected to surgeries done in Matamoros, Mexico, under the influence of epidural anesthesia. Health officials are quite concerned about this outbreak, so a coordinated international response is needed to manage and limit it.
Background
Fungal meningitis, although rare, poses a significant threat to individuals’ health due to its potential to cause severe inflammation around the brain and spinal cord. The infection occurs when fungal pathogens gain access to the central nervous system, leading to an inflammatory response and subsequent tissue damage.
Infection control practices are crucial in preventing the transmission of fungal pathogens during medical procedures. Proper sterilization techniques, strict adherence to aseptic protocols, and the use of sterile equipment are essential to minimize the risk of fungal contamination. However, when these infection control practices are compromised, such as inadequate sterilization or contamination of medical devices, the chance of introducing fungal pathogens into the body increases significantly.
Once fungal pathogens enter the body, they can reach the central nervous system through various routes. In the case of epidural anesthesia procedures, the pathogens may gain access to the spinal cord and brain through the epidural space. This can occur when contaminated needles, catheters, or medications are used during the procedure.
Fungal meningitis differs from its bacterial and viral counterparts in terms of its development and progression. Fungal infections generally have a longer incubation period, meaning it takes a longer time for symptoms to manifest after exposure. This delayed onset can make it challenging to identify and diagnose fungal meningitis promptly.
When infection control practices are compromised, the risk of fungal contamination increases, especially for immunocompromised individuals. People with weakened immune systems, such as those with HIV/AIDS, undergoing chemotherapy, or receiving organ transplants, are more susceptible to developing fungal infections, including fungal meningitis. Therefore, it is crucial to maintain stringent infection control practices, particularly when treating vulnerable patient populations.
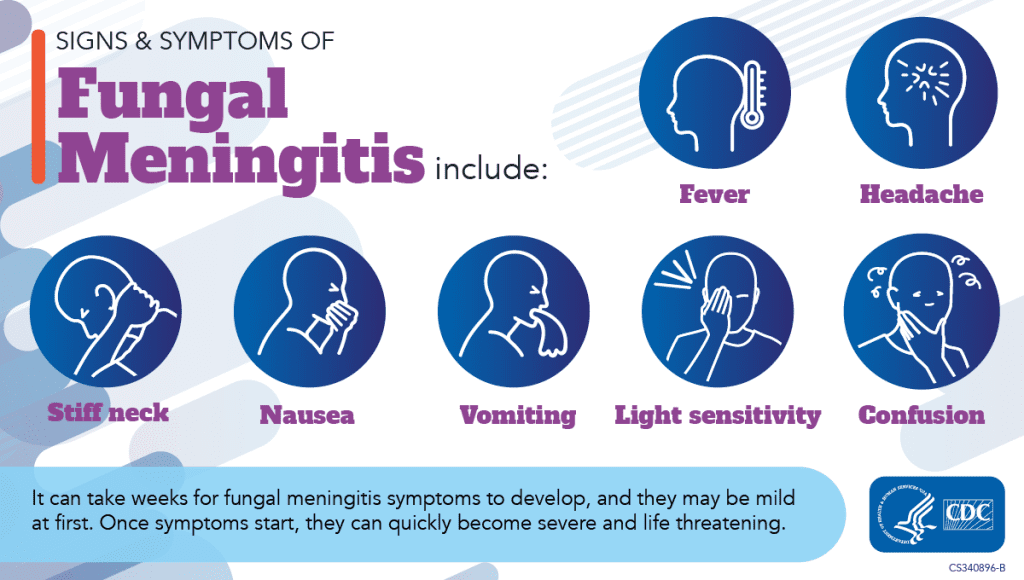
The consequences of fungal meningitis can be severe. The inflammation around the brain and spinal cord can lead to a range of debilitating symptoms, including fever, headache, neck stiffness, nausea, vomiting, sensitivity to light (photophobia), and confusion. If left untreated, fungal meningitis can rapidly progress, leading to life-threatening complications such as seizures, coma, and even death.
Matamoros Meningitis Outbreak
State and municipal health departments in the United States, the CDC, and Mexican health officials are all working hard to contain the frightening spread of fungal meningitis among patients who received epidural anesthetic treatments in Matamoros, Tamaulipas, Mexico. Two facilities, River Side Surgical Center and Clinica K-3, were found to be the outbreak’s focal points and were consequently closed on May 13, 2023.
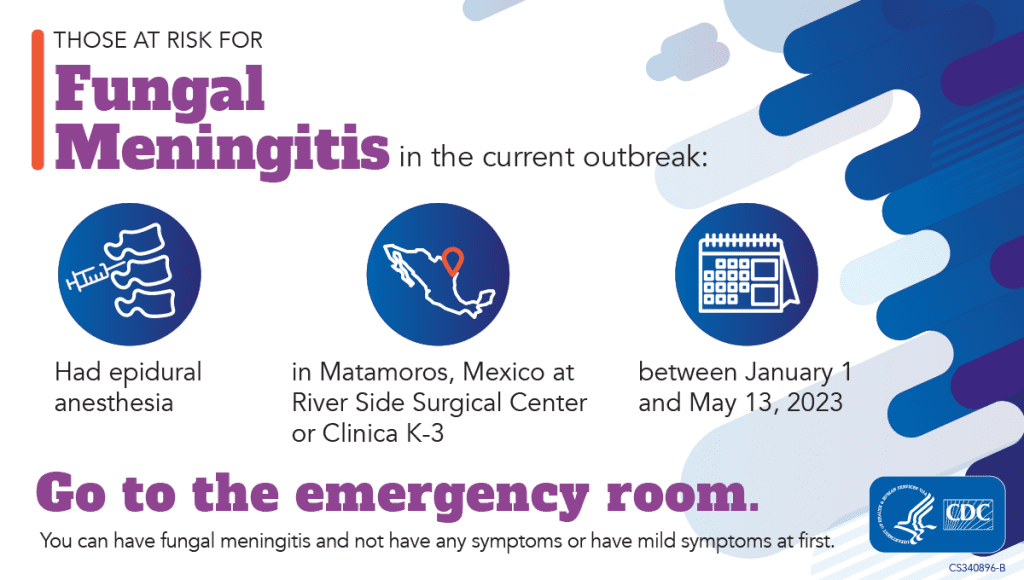
Information for Those at Risk
A risk of fungus meningitis exists for patients who underwent treatments at the indicated clinics between January 1 and May 13, 2023. Even if they are currently symptom-free, it is critical for them to contact the local emergency room right away for evaluation. The key to increasing survival rates is early screening and therapy. Fever, headache, stiff neck, nausea, vomiting, sensitivity to light, and confusion are among the signs of fungus meningitis. It is crucial to remember that symptoms might take weeks to appear, and some infected people may initially show only minor symptoms or none at all.

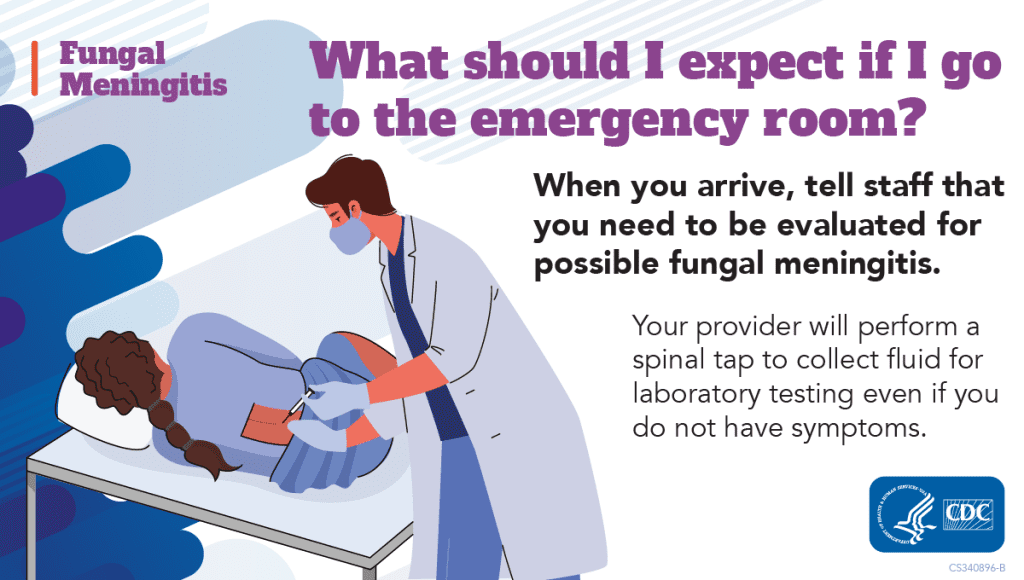
What to Expect During Evaluation
During the evaluation at the healthcare facility, a lumbar puncture (spinal tap) will be conducted to collect cerebrospinal fluid for laboratory testing. If diagnosed with fungal meningitis, patients will be treated with antifungal medications for at least two weeks in the hospital. Additionally, a follow-up antifungal treatment plan for three to six months will be prescribed to ensure complete eradication of the infection.
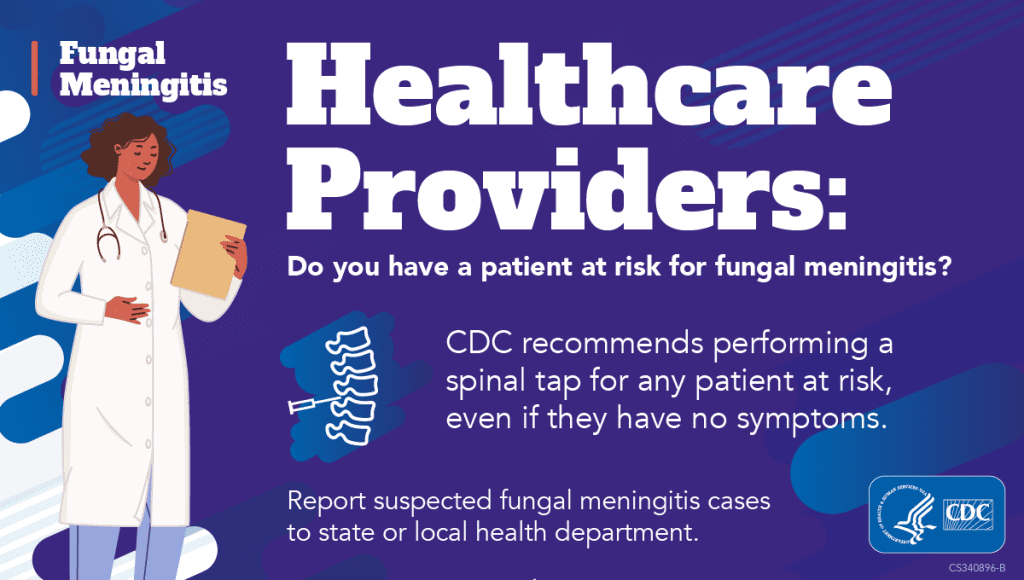
Recommendations for Healthcare Providers
Healthcare providers are encouraged to report any suspected cases of fungal meningitis to their respective state or local health department. Interim diagnostic and management recommendations have been provided by the CDC, offering a comprehensive guide for clinicians treating patients who underwent epidural anesthesia procedures in Matamoros. Notably, asymptomatic patients with potential exposure should also be tested to prevent severe complications, as the latency of symptom onset provides an opportunity for early intervention.
One-page summary of interim recommendations
Clinical diagnosis and treatment algorithm
Findings and Investigations
Key findings from investigations include the detection of elevated levels of Beta-D-glucan in cerebrospinal fluid samples of some U.S. patients and the presence of fungal signals consistent with the Fusarium solani species complex. The CDC and partner institutions are continuing to investigate the source of exposure during the affected medical procedures, while also exploring the potential involvement of other clinics.
CDC’s Response and Ongoing Efforts
The CDC’s response to the outbreak has been comprehensive and multi-faceted. It includes the publication of a Travel Health Notice, the distribution of Health Alert Notices, collaboration with the Mycoses Study Group to develop clinical resources and webinars, and ongoing outreach to potentially impacted patients. Additionally, the CDC is working with Mexican colleagues to investigate the outbreak’s source and disseminate critical information to healthcare professionals, the public, and partners.
Conclusion
Fungal meningitis is a rare but dangerous infection that causes inflammation around the brain and spinal cord. The infection primarily occurs when infection control practices during medical procedures are compromised. The fungal meningitis outbreak associated with epidural anesthesia in Matamoros, Mexico, remains a significant public health concern. The collaborative efforts of the CDC, Mexican health authorities, and state and local health departments in the United States are crucial in containing and managing the outbreak. Timely testing, early treatment, and heightened awareness among healthcare providers and the public will play a pivotal role in minimizing the impact of this life-threatening infection.
Source: Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of Healthcare Quality Promotion (DHQP)
Subscribe
to get our
LATEST NEWS
Related Posts

Infectious Diseases & Vaccinology
Harnessing IgA: A Breakthrough in HIV Vaccine Innovation
A vaccine eliciting strong IgA responses could revolutionize HIV prevention by protecting the virus’s primary entry points.
Infectious Diseases & Vaccinology
Prostate Cancer Precision-Targeting: The Promise and Challenges of Vaccine Therapies
The future of prostate cancer vaccines lies in combination therapies that harness the strengths of multiple modalities.