Hemophilia is a rare bleeding disorder that affects blood clotting. It is a hereditary disorder that occurs more commonly in males than females. Hemophilia is caused by a deficiency of clotting factors VIII (hemophilia A) or IX (hemophilia B) in the blood. The disease is known to have an impact on the quality of life of affected individuals and their families. In this blog post, we will explore the etiology, pathophysiology, history and physical manifestations, evaluation, treatment and management, differential diagnosis, prognosis, complications, and current research endeavors related to hemophilia.
Etiology & History
Hemophilia is a hereditary disorder that is caused by a mutation in the genes that produce clotting factors VIII or IX. The genes responsible for hemophilia are located on the X chromosome, which means that males are more likely to be affected than females. Females have two X chromosomes, and if one of them carries the mutated gene, the other healthy X chromosome can compensate for the deficiency. However, females with one mutated gene are carriers and can pass the mutation on to their children. Hemophilia is an X-linked recessive disorder, which means that a male child has a 50% chance of inheriting the disease from his carrier mother.
The history of hemophilia dates back to ancient times. It was first described in the Talmud in the second century AD. In the 1800s, Queen Victoria of England was a carrier of the hemophilia gene, and several of her descendants were affected by the disease.
Pathophysiology & Physical Manifestations
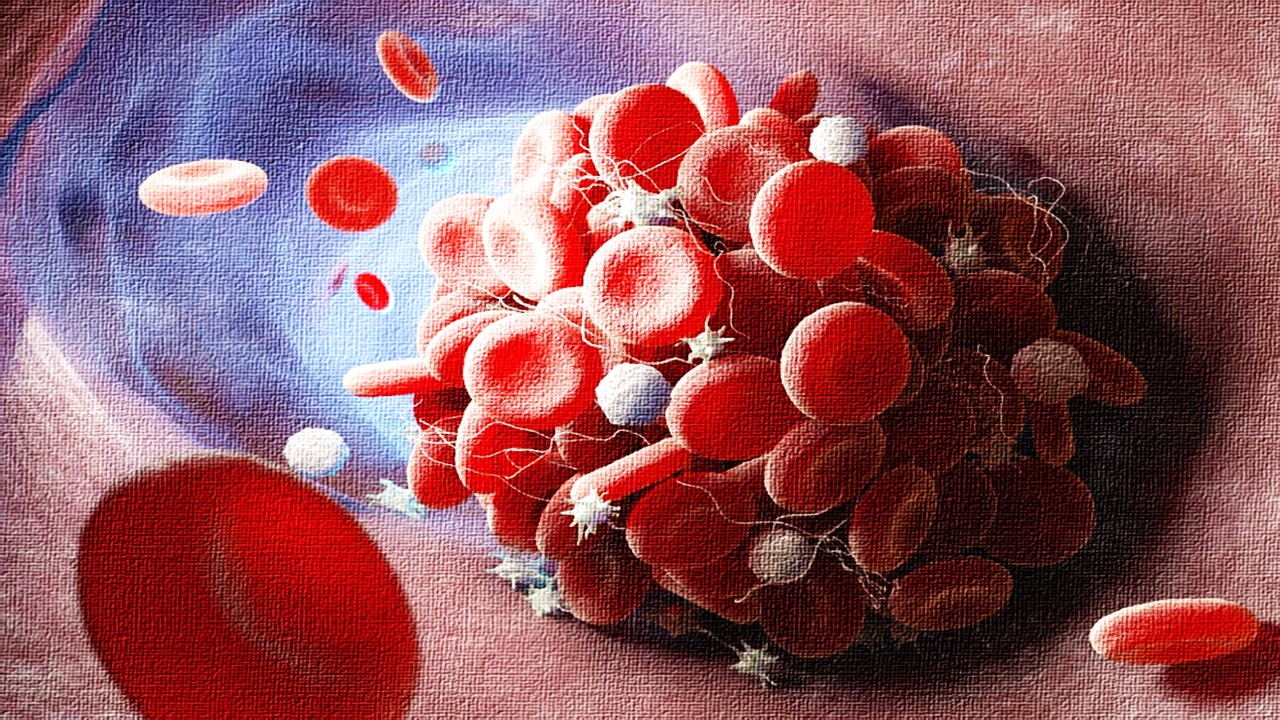
Hemophilia is a bleeding disorder that affects blood clotting. The clotting process involves several steps, including the activation of clotting factors, platelets, and the formation of a fibrin clot. Hemophilia occurs when there is a deficiency of clotting factor VIII or IX in the blood. As a result, the clotting process is impaired, and individuals with hemophilia bleed longer and more severely than individuals without the disease. Bleeding episodes can occur spontaneously or after an injury or surgery. Hemophilia can range from mild to severe, depending on the level of clotting factor deficiency.
The physical manifestations of hemophilia include prolonged bleeding after injury, surgery, or tooth extraction, joint pain and swelling, easy bruising, and spontaneous bleeding into muscles or organs.
Evaluation
The diagnosis of hemophilia is based on a physical examination, medical history, and laboratory tests. The laboratory tests include clotting factor assays, which measure the levels of clotting factors VIII and IX in the blood, and a bleeding time test, which measures the time it takes for a small cut to stop bleeding. Genetic testing can also be done to confirm the diagnosis and identify carriers of the disease.
Treatment and Management
The treatment of hemophilia involves replacement of the deficient clotting factor. Clotting factor concentrates can be given intravenously to replace the missing factor and prevent bleeding episodes. The frequency and dose of treatment depend on the severity of the disease. For mild hemophilia, treatment may only be necessary during surgical or dental procedures. For severe hemophilia, prophylactic treatment may be necessary to prevent bleeding episodes. In addition to factor replacement therapy, other treatments include desmopressin, which stimulates the release of von Willebrand factor, a protein that helps with blood clotting, and antifibrinolytic drugs, which help to stabilize blood clots.
Differential Diagnosis
The differential diagnosis of hemophilia includes other bleeding disorders, such as von Willebrand disease, platelet function disorders, and liver disease. A careful evaluation of the medical history, physical examination, and laboratory tests can help to distinguish between these conditions.
Prognosis and Complications
The prognosis of hemophilia depends on the severity of the disease. Individuals with mild hemophilia may have few complications, while those with severe hemophilia may experience recurrent bleeding episodes that can lead to joint damage, muscle and tissue damage, and even life-threatening bleeding in the brain or other organs. With proper treatment and management, however, individuals with hemophilia can lead normal, healthy lives.
Current Research Endeavors
Advancements in gene therapy are providing new hope for individuals with hemophilia. Gene therapy involves the insertion of a healthy copy of the clotting factor gene into the patient’s cells to produce a permanent source of the missing factor. Clinical trials have shown promising results, and gene therapy may soon become a viable treatment option for individuals with hemophilia.
In addition to gene therapy, researchers are also exploring new ways to improve the delivery of clotting factor concentrates and developing new treatments that target the underlying mechanisms of hemophilia. These advancements in hemophilia research hold the promise of improving the quality of life for individuals with hemophilia and their families.
Subscribe
to get our
LATEST NEWS
Related Posts

Pathophysiology & Experimental Medicine
Autism Disentangled: FOXG1 Drives Neural Imbalance in the Developing Brain
If FOXG1 overexpression can be modulated, either genetically or pharmacologically, it may be possible to correct the neurodevelopmental imbalances underlying ASD.
Pathophysiology & Experimental Medicine
Adaptive Interactions: How Stimuli-Responsive Materials Revolutionize Cellular Studies
Stimuli-responsive materials revolutionize cellular dynamics research by replicating ECM adaptability, unlocking insights into cell behavior and regulation.

Pathophysiology & Experimental Medicine
Eternal Lip Layers: Unlocking the Human Keratinocyte Potential
The lips, long celebrated for their role in communication and aesthetics, now stand at the forefront of scientific innovation.
Pathophysiology & Experimental Medicine
Thrombosis-Free Surfaces: Preventing Blood Clot Formation on Medical Implants Through Selective Protein Interactions
The synthesis and mechanisms of SPI coating are explored, evaluating its potential to overcome the limitations of traditional antifouling surfaces.
Read More Articles
Mini Organs, Major Breakthroughs: How Chemical Innovation and Organoids Are Transforming Drug Discovery
By merging chemical innovation with liver organoids and microfluidics, researchers are transforming drug discovery into a biologically precise, patient-informed, and toxicity-aware process.
Tetravalent Vaccines: The Power of Multivalent E Dimers on Liposomes to Eliminate Immune Interference in Dengue
For the first time, a dengue vaccine candidate has demonstrated the elusive trifecta of broad coverage, balanced immunity, and minimal enhancement risk,