Autoimmune diseases represent a unique challenge to the immune system, as they arise from a breakdown in self-tolerance, leading to the body’s own defense mechanisms erroneously mounting an attack against its own healthy tissues. This intricate interplay between immune dysfunction and autoimmune diseases unfolds through an intricate web of immunological processes, involving multiple immune cell types, intricate signaling networks, and an array of molecular interactions. An in-depth exploration of the complexity behind these conditions not only sheds light on the mechanisms underlying immune dysregulation but also reveals potential avenues for immune reconstitution and therapeutic intervention.
Genetic Predisposition and Autoimmune Susceptibility
The pathogenesis of autoimmune diseases involves a multifaceted interplay between genetic predisposition, environmental triggers, and dysregulated immune responses. Genetic factors contribute significantly to autoimmune susceptibility, with certain gene variants predisposing individuals to the development of specific autoimmune disorders. These genetic elements impact critical aspects of immune regulation, such as antigen presentation, immune cell development, and signaling pathways, thereby influencing the threshold for immune activation and self-recognition.
Environmental Triggers and Autoimmune Activation
Environmental triggers, including infections, drugs, and lifestyle factors, play a crucial role in initiating and exacerbating autoimmune responses. Molecular mimicry, where microbial antigens bear similarities to self-antigens, can lead to the activation of autoreactive immune cells. Environmental toxins and drugs can modulate immune responses, promoting dysregulation and altering immune cell function. Furthermore, hormonal and psychosocial factors have been implicated in the modulation of immune responses and the development of autoimmune diseases.
Dysregulation of Immune Tolerance Mechanisms
Central to the pathogenesis of autoimmune diseases is the dysregulation of immune tolerance mechanisms, which normally prevent the immune system from attacking self-antigens. Tolerance mechanisms involve a delicate balance between immune activation and regulation, with intricate networks of immune cells and regulatory molecules acting in concert to maintain immune homeostasis. Dysfunctions in immune checkpoints, such as defects in regulatory T cells (Tregs) or abnormalities in co-stimulatory and co-inhibitory pathways, can disrupt this balance and precipitate autoimmunity.
Immune Cell Types in Autoimmune Pathogenesis
Within the context of autoimmune diseases, a myriad of immune cell types contribute to the pathogenic immune response. Autoreactive T cells, including CD4+ helper T cells and CD8+ cytotoxic T cells, recognize self-antigens presented by antigen-presenting cells and orchestrate immune responses against healthy tissues. B cells, in turn, produce autoantibodies that target self-antigens, further exacerbating tissue damage through complement activation, immune complex deposition, and inflammation. Additionally, innate immune cells, including dendritic cells, macrophages, and natural killer cells, actively participate in the pathogenesis of autoimmune diseases by promoting immune activation and inflammation.
Targeting Signaling Pathways and Molecular Networks
The intricate signaling pathways and molecular networks involved in autoimmune diseases offer potential targets for immune reconstitution and therapeutic intervention. Cytokines, such as interleukins and interferons, play critical roles in shaping immune responses and can be modulated to restore immune balance. Small molecules and biologics targeting immune checkpoints, such as CTLA-4, PD-1, or PD-L1, have shown promise in reestablishing self-tolerance and dampening autoimmunity. Furthermore, therapies that selectively deplete autoreactive immune cells, such as monoclonal antibodies targeting B cells or T cells, have demonstrated efficacy in certain autoimmune disorders.
Unraveling the Molecular Landscape of Autoimmune Diseases
Advances in our understanding of the immunogenetics underlying autoimmune diseases, coupled with sophisticated technologies like high-throughput sequencing and single-cell analysis, provide unprecedented opportunities to unravel the intricacies of immune dysregulation. Integration of large-scale omics data, bioinformatics, and computational modeling allows for the comprehensive exploration of the molecular landscape of autoimmune diseases, paving the way for the identification of novel therapeutic targets and personalized treatment strategies.
In summary, autoimmune diseases arise from a complex interplay between genetic predisposition, environmental triggers, and dysregulated immune responses. Understanding the intricate immunological mechanisms underlying these disorders is crucial for developing targeted therapies and strategies for immune reconstitution. The evolving field of immunology, driven by cutting-edge research and interdisciplinary collaborations, holds the promise of unlocking new avenues for unraveling the complexity of autoimmune diseases, ultimately leading to improved diagnostic tools, tailored therapies, and enhanced management of these challenging conditions.
Engr. Dex Marco Tiu Guibelondo, BS Pharm, RPh, BS CpE
Subscribe
to get our
LATEST NEWS
Related Posts

Immunology & Oncology
The Silent Guardian: How GAS1 Shapes the Landscape of Metastatic Melanoma
GAS1’s discovery represents a beacon of hope in the fight against metastatic disease.
Immunology & Oncology
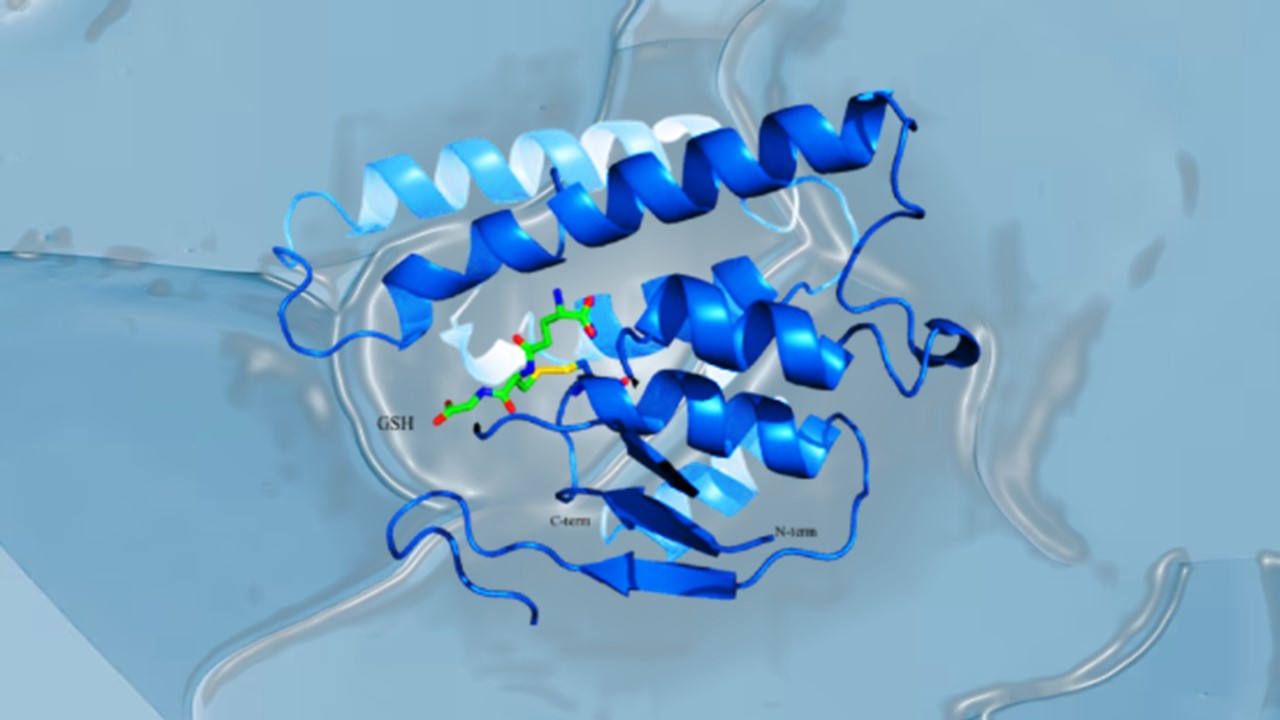
Resistance Mechanisms Unveiled: The Role of Glutathione S-Transferase in Cancer Therapy Failures
Understanding this dual role of GSTs as both protectors and accomplices to malignancies is central to tackling drug resistance.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.
Designing Better Sugar Stoppers: Engineering Selective α-Glucosidase Inhibitors via Fragment-Based Dynamic Chemistry
One of the most pressing challenges in anti-diabetic therapy is reducing the unpleasant and often debilitating gastrointestinal side effects that accompany α-amylase inhibition.