The pharma industry is constantly changing with more and more drugs and treatments becoming available each year. As science and tech advance, worries about drug safety grow, especially when it comes to people having adverse events (AEs) – this is known as pharmacovigilance (PV). Pharma companies have to pull together info from multiple sources, which increases the chances of them not meeting regulatory requirements. This leads to a dramatic rise in the cost of clinical research and development, sub-par clinical trial implementation and delays in getting new drugs out there. Tata Consultancy Services’ Advanced Drug Development (TCS ADD™) helps create digital systems, simplifies data and encourages innovation in clinical trials so that drugs can be released quickly.
The Need for Artificial Intelligence in Pharmacovigilance
There’s a lot of buzz surrounding the use of artificial intelligence (AI) for drug creation and maintenance, including pharmacovigilance. The FDA has a wide definition for PV, covering individual case safety reports (ICSRs), pharmacoepidemiologic studies, registries, and other methods. They’re looking into using AI for these areas but it’s not quite ready for widespread implementation yet. We’re focusing here on the use of AI to process data from multiple sources to detect adverse events, prep them into ICSRs, and then report and evaluate them.
We’re focusing on this because new safety issues pop up all the time after a drug is approved, and ICSRs have been good at recognizing these issues. Plus, there are lots more data sources to check out now, so it’s a lot of work for the safety experts we have. The coronavirus pandemic has added to this, too. Governments around the world require ICSRs, and it makes things more efficient to do it the same way. But we still don’t know if population-based data sources can replace ICSRs. So, ICSRs will probably still be important in the future for recognizing rare safety signals. Modifying ICSRs can help a bit, but it won’t be enough to keep up with all the data sources and ICSRs.
Model for AI Readiness
When figuring out if an AI algorithm is ready to go, there’s a lot to think about. Performance – like validity, generalizability, no bias, and how it’ll work in the real world – is probably the most important thing, but you also need good documentation, transparency, explainability (like why it made certain predictions), quality control with real-world data and monitoring, and a way to keep track of any changes. There’s still a lot of work to do to make sure AI follows best practices for data management, feature extraction, training, interpretability, evaluation, and documentation. We need to standardize the terminology used in AI frameworks too, so everyone’s on the same page. All these steps need to be taken so AI can reach its full potential.
The Pharmacovigilance Process
When you submit an ICSR, you’ll need to provide info on the patient, the adverse event, the suspect medication, and the person reporting it. If it’s a company that holds the license or application for the drug, then they’ll also need to be included. The FDA has regulations that require ICSRs to be created from any source, including info from marketing, clinical investigations, studies, scientific literature, and unpublished papers. Once the company has figured out if it needs to be reported or not, then the FDA will start evaluating and processing the case. This is split between the industry and the FDA.
Case Processing
The four steps of case processing have been described as intake, evaluation, follow-up, and distribution, with numerous subprocesses for each step. The four criteria—an identifiable reporter, an identifiable patient, an adverse response, and a questionable product—that, when present, indicate that an ICSR must be produced and submitted—are identified during the intake of cases that may require submission to the FDA. The minimal requirements for an ICSR are these four components, however where available, an ICSR must also include all pertinent information.
The identification of additional regulatory categories, such as the seriousness of the AE, whether the AE is already included in the FDA prescribing information for the product (expectedness), and, for some ICSRs (AEs from a study), the likelihood of a causal association, involves further stages. The information in the report, the product label, and the information’s source all play a role in these decisions. A report’s transmission to regulators includes a follow-up to collect any missing information.
The International Council for Harmonization (ICH) E2B guideline now serves as the primary standard for ICSR transmission from industry to regulatory authorities. It’s significant that this standardized includes both structured fields for numerous data pieces as well as an unstructured narrative account of the case, which frequently contains important information that isn’t documented in the structured data.
Case Causality Assessment
Case causality assessment, which determines whether the drug is likely to have contributed to the reported adverse event, is done by both the FDA and the industry. Expert judgment and broad introspection continue to be the mainstays of ICSR causality assessment. The ICSR case assessment workflow is not fully standardized to the level needed for computation, despite the fact that the FDA mandates that businesses have “written procedures for the surveillance, receipt, evaluation, and reporting of post-marketing adverse drug experiences” and has established best practices and workflows for its own work.
The necessity for expert judgment and flexibility must be acknowledged in any attempt to standardize the workflow for computing purposes. To meet this goal, AI systems must be able to comprehend both the individual activities carried out and how they are subsequently put together into a cognitive framework for evaluation to support human efforts, in a variety of complex and hard-to-describe scenarios.
Getting the Right Human and AI Balance
The main problem of putting a “human-in-the-loop” is to assure quality without sacrificing the efficiency achieved by the AI algorithm if an algorithm does not reach the performance levels necessary for full automation. In other words, a human expert shouldn’t perform tasks that a machine can perform effectively and efficiently, and a machine shouldn’t perform (poorly) tasks that a human expert can complete successfully.
A risk-based approach, where effort is proportional to the implications of misclassification on the overall evaluation goals, careful application of algorithm development principles, or the use of formal confidence metrics, are general considerations for the qualities of quality assurance that could be applied to a human-in-the-loop approach to an imperfect AI system.
Tata Consultancy Services ADD™ Safety Platform
The COVID-19 pandemic has made the past three years difficult for life sciences organizations. There is a greater public awareness of the safety of pharmaceutical products, an increase in the number of safety instances, and an unprecedented demand for information and replies. As a result, in order to operate and manage patient safety data effectively and efficiently, the pharmacovigilance approach has been compelled to change, innovate, embrace efficient solutions, and use smart technology.
During the 5th Global Annual Achievement Awards for Artificial Intelligence, Tata Consultancy Services ADD™ Safety won ‘The Best Technical Implementation for AI’ for reimagining pharmacovigilance. TCS ADD™ Safety employs source-agnostic automation to extract, derive, and infer data. It allows for modular deployment with an interface to safety database. TCS ADD™ Safety has E2B and non-E2B field automation to reduce manual intervention. Finally, it has learning management with identified learnings and performance management module for case reconciliation.
“In order to accelerate clinical R&D and launch drugs faster to market, it is extremely important that science is complemented with easy-to-implement technology that is powered by artificial intelligence, data-driven smart analytics, and Internet of Things,” emphasizes Rachna Malik, Global Head of Tata Consultancy Services ADD™ Platforms.
TCS ADD™ enables quicker decision-making with real-time access to data and faster drug registration with its adaptive trial design feature. With improved data quality because of its advanced analytics, TCS ADD™ is surely the to-go unified platform for sites, patients, and regulators.
So far, TCS ADD™ has been implemented in more than 50,000 sites globally. It has supported more than 700 clinical trials. It has been 100 percent compliant with FDA regulations while improving efficiency by 40 percent and reducing drug monitoring efforts by 80.
The implementation of TCS ADD™ Safety specifically shows 96 percent improvement of accuracy in processing adverse events. A 40 percent efficiency gain in case processing efforts and 30 percent cost savings in end-to-end case processing are the safety platform’s additional advantages. Compliance to regulatory timelines is 100 percent guaranteed upon usage of TCS ADD™ Safety with 50 percent reduction in quality control efforts and 70 percent reduction in manual efforts.
“With the TCS ADD™ platforms, life sciences companies across the world can harness the power of AI and analytics to accelerate the development of new, more effective drugs for patients. TCS ADD™ Safety helps transform safety case processing and meet business and regulatory requirements effectively and efficiently,” Malik adds.
TCS ADD Virtual Event for Pharmacovigilance
TCS ADD™ Safety was glad to organize a panel discussion with industry representation that concentrated on the critical elements that facilitate the easy implementation of smart pharmacovigilance and the contribution of AI to patient safety. The TCS ADD™ Safety panelists at the virtual event also talked about how a technology-led strategy might make it possible to process safety cases in pharmacovigilance. The following is a high-level overview of the themes covered at the virtual event:
(1) Using AI as a scalable method to address the amount of safety cases;
(2) Using AI to manage complexity in safety reports;
(3) Improving pharmacovigilance compliance with artificial intelligence;
(4) Improving quality and accuracy while increasing efficiency; and
(5) Sharing real-world examples of implementing artificial intelligence in pharmacovigilance, along with lessons learned and future directions.
TCS ADD™ Safety has onboarded, revered panelists serving as virtual event speakers, who have been responsible for transforming pharmacovigilance in their organizations through industry-first initiatives. The industry expert speakers are as follows:
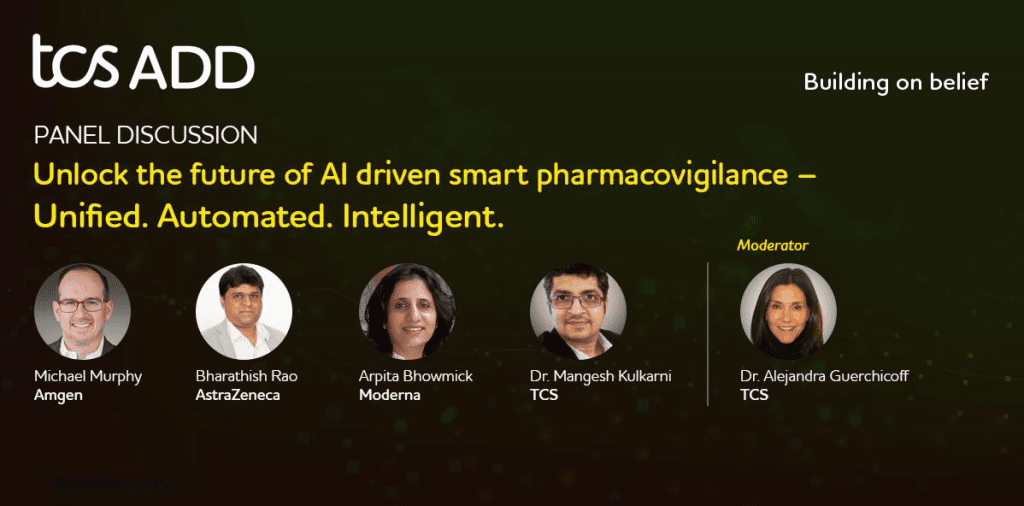
(1) Michael Murphy, Executive Director and Head of Pharmacovigilance Operations, Amgen;
(2) Bharathish Rao, Associate Director, Patient Safety Systems (CMO Organization), AstraZeneca;
(3) Arpita Bhowmick, Global Director, Omni Channel Contact Center Technology, Moderna; and
(4) Dr. Mangesh Kulkarni, Medical Director and Head of PV, TCS.
The event was moderated by TCS ADD™ Safety Industry Leader at TCS, Dr. Alejandra Guerchicoff.
Click the link to check out the TCS virtual event: http://bit.ly/3JfZcVb.
Subscribe
to get our
LATEST NEWS
Related Posts

Pharmacovigilance
Complexity of Clinical Decision Support Systems
In today’s healthcare, where choices can make all the difference, CDSSs shine as trusted guides.

Pharmacovigilance
Iatrogenic Disorders: A Hidden Risk of Medical Treatment
“All men make mistakes, but a good man yields when he knows his course is wrong, and repairs the evil. The only crime is pride.”— Sophocles, Antigone”
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.













