For a long time, the pharmaceutical industry has relied on monolithic substances to deliver therapeutic outcomes. These substances would have to fulfill targeting criteria, pharmacokinetics and pharmacodynamics all on their own – not only did they have to deliver the desired effect, but they also had to deliver it to the right part of the body, for the right time. While this approach has yielded many successes, the rise of multispecific drugs promises to revolutionize the number of substances we can use. Unlike traditional active ingredients, multispecific drugs can benefit from enhanced targeting and therapeutic impact – through the combination of diverse agents. We explore a brief history of the modality, and the possibilities for its future.
The Waves of Innovation
In the industry, the largest frame-shifts in drug development have often been referred to as waves of innovation – describing revolutions in drug discovery. The first wave, experienced in the 20th century, was the random discovery of active ingredients from biological sources and extracts, followed by structure-based and rational drug discovery in the 1970s – which to this day remains the most common approach. The third wave, the advent of recombinant protein-based treatments, is still growing.
Experts believe the growth of multispecific drugs will be the fourth wave among these, with transformational potential for the industry. There are multiple types of multispecific drugs – classified based on their mode of action or component molecules. These include antibody-drug conjugates, antibody-cytokine combinations, small-molecule chimeras such as PROTACs (proteolysis targeting chimeras), and others. We will briefly examine these three types here – with examples from investigational or marketed products.
Antibody-Drug Conjugates
Cancer is one of the leading causes of death worldwide – and the tissues that cause the disease are often difficult to target pharmaceutically without affecting healthy tissues. With these two premises in mind, it is not hard to understand why oncology treatments have some of the lowest standards for safety profiles across therapeutic areas: often, there is a direct trade-off between toxicity and efficacy. Antibody-drug conjugates promise to change that – by enabling much higher degrees of specificity, limiting off-site effects, and allowing us to use cytotoxic agents that would otherwise be non-viable because of their toxicity.
The first multispecific drug to be approved was Gemtuzumab ozogamicin, marketed as Mylotarg by Pfizer. The agent was used to treat acute myelogenic leukemia. Its early approval in 2000 signaled the potential for this specific class of multispecifics – known as antibody-drug conjugates. However, the drug faced a troubled journey – with a withdrawal from the market in 2010 after studies found its potential for veno-occlusive disease. It gained re-approval later on, based on new clinical trials and alternative dosing schedules to reduce toxicity.
The market for antibody-drug conjugates is expected to continue growing, with market size expected to surpass $25b by 2028. Over 18 agents have been approved so far – a marked increase from the three that were in the market in 2017. The use of antibody-drug conjugates is also expanding beyond oncology – with AbbVie having begun investigations of a candidate agent, ABBV-3373, for the treatment of rheumatoid arthritis. The FDA has also published guidance specifically tailored for the development of antibody-drug conjugates, showing that the technology is here to stay.
Antibody-Cytokine Fusions
Cytokines are one of the most potent parts of the immune system’s arsenal – able to modulate and promote immune responses. Cytokines are small proteins, and were one of the first immune-based treatments to be tested against cancer. This started with the approval of Interleukin-2 for the treatment of metastatic renal cell melanoma, due to its ability to produce complete responses in some patients.
However, systemic, non-localized treatment with cytokines can have devastating side-effects – in addition to not being guaranteed to lead to the desired end-points. Similarly to antibody-drug conjugates, antibody-cytokine fusions aim to localize the effect of cytokines to limit toxicity. Though none have yet entered the market, products are currently being investigated for ulcerative colitis, rheumatoid arthritis, soft-tissue sarcomas, melanomas, and other cancer indications.
Cytokines have been noted for their potential in combination therapies – which has led to the development of even antibody-cytokine-drug conjugates. The cytokine in the trifunctional conjugate is expected to stimulate the immune response, while the drug delivers cytotoxic effects and the antibody localizes the drug appropriately. Other developments in the cytokine space also involve the fusion of cytokines to proteins that are naturally degraded when the cytokine finds itself in its target environment, rather than using an antibody for localization. We talked to Randi Isaacs from Werewolf to find out more about their own take on this technology.
Proteolysis Targeting Chimeras
Small-molecule chimeras combine multiple, typically two, active domains through a linker. The entire category of small molecule chimeras includes a diverse array of potential agents, defined by the class of protein they aim to target. Proteolysis Targeting Chimeras (PROTACs), which achieve protein degradation by bringing a target protein into the ubiquitination pathway of the cell, are the modality of small-molecule chimeras which has seen the most progress so far. However, other classes – such as Ribonuclease Targeting Chimeras (RIBOTACs) – also exist.
PROTACs, compared to classical small-molecule inhibitors, promise to bring about effective and more durable results at lower dosages, while also demonstrating higher selectivity and fewer toxicities. Conjointly, the more targeted nature of PROTACs – which does not rely on catalytic active sites on the target proteins – also has the potential to open up new targets for treatment. PROTACs first entered the clinic in 2019, targeting androgen and estrogen receptors. While no small-molecule chimeras have yet entered the market, the technology shows significant potential – we talked to Guido Koch from Amphilix to obtain an insider’s point of view.
As pharmaceutical treatments become more sophisticated, it is inevitable that progress towards better targeted therapies will be a priority. The development of multispecific drugs allows us to use substances we know are effective – but are otherwise unsuitable for use on their own; additionally, they open up new horizons for targeting previously undruggable targets. But most importantly, they promise to deliver safer, less toxic treatments. Antibody-Drug Conjugates have made the biggest inroads – but other, equally exciting technologies follow close behind.
Nick Zoukas, Former Editor, PharmaFEATURES
Join Proventa International’s Medicinal Chemistry Strategy Meeting in Boston to hear more on the latest development in the field of multispecific drug development. Participate in closed door roundtable discussions that aim to facilitate scientific discourse between key stakeholders and establish new collaborations, and exchange ideas on cutting-edge topics from throughout the field.

Subscribe
to get our
LATEST NEWS
Related Posts

Medicinal Chemistry & Pharmacology
Aerogel Pharmaceutics Reimagined: How Chitosan-Based Aerogels and Hybrid Computational Models Are Reshaping Nasal Drug Delivery Systems
Simulating with precision and formulating with insight, the future of pharmacology becomes not just predictive but programmable, one cell at a time.

Medicinal Chemistry & Pharmacology
Coprocessed for Compression: Reengineering Metformin Hydrochloride with Hydroxypropyl Cellulose via Coprecipitation for Direct Compression Enhancement
In manufacturing, minimizing granulation lines, drying tunnels, and multiple milling stages reduces equipment costs, process footprint, and energy consumption.

Medicinal Chemistry & Pharmacology
Decoding Molecular Libraries: Error-Resilient Sequencing Analysis and Multidimensional Pattern Recognition
tagFinder exemplifies the convergence of computational innovation and chemical biology, offering a robust framework to navigate the complexities of DNA-encoded science
Read More Articles
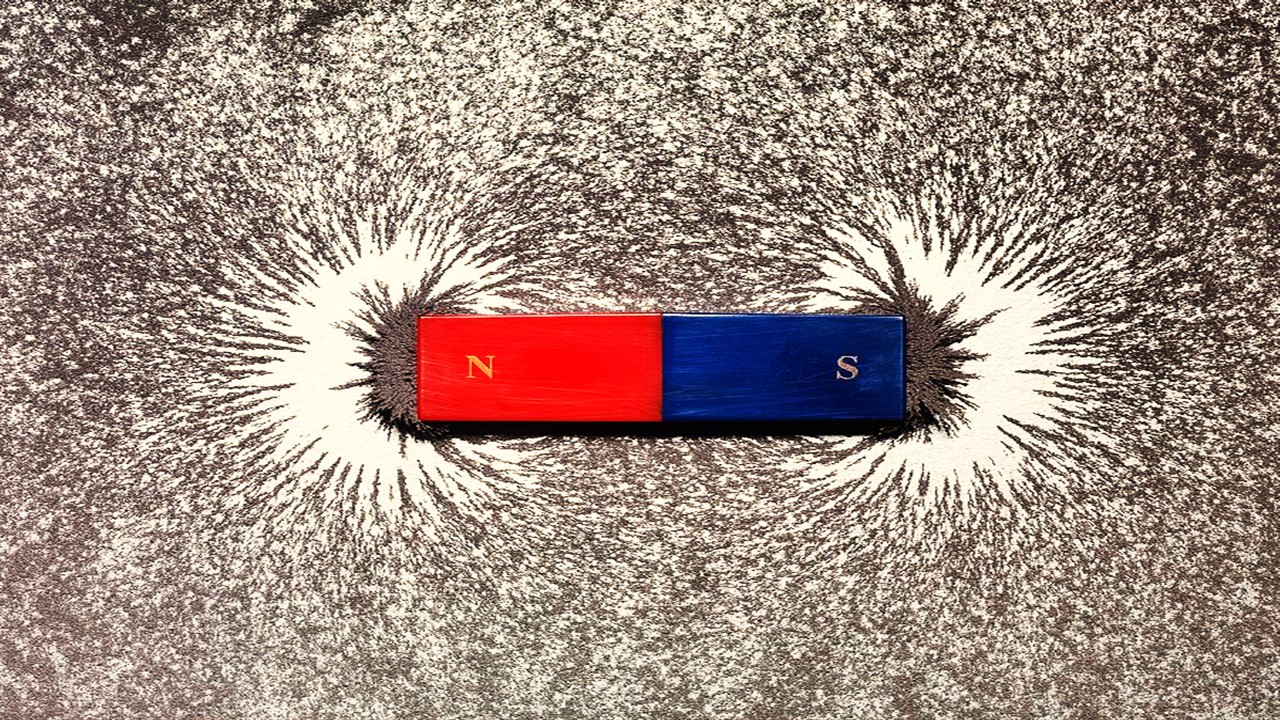
Magnetic Nanoengineering: Overcoming Biological Variability and Enhancing Therapeutic Precision
The future of nanomedicine lies in harmonizing precision, accessibility, and ecological responsibility, ushering in an era where therapies are tailored to individual biological landscapes.