Cancer diagnostics and biomarker profiling are crucial for providing solutions to key questions for oncological treatments. For clinical trials and therapies to improve, we require vast amounts of data regarding individual biomarkers and tumour progression. Presently, the best way to obtain this data is through biopsies – which can be very invasive, limiting the number and frequency of procedures that can be performed. Liquid biopsies, particularly harnessing the power of circulating tumour DNA (ctDNA), promise to revolutionize the field and bring about a deeper understanding of cancer at the individual level, enabling more precise treatment.
ctDNA and its Applications
ctDNA is shed by dying cancer cells into the bloodstream – and can therefore be picked up by non-invasive blood tests. ctDNA is generally more fragmented than non-mutant cell-free DNA (cfDNA), and has a relatively short half life of 7 hours. Despite these limitations, using next-generation sequencing for ctDNA can provide a snapshot of the tumour genome. Distinguishing ctDNA from normal, non-mutant cell-free DNA (cfDNA) does remain a challenge, although improvements in sequence technology are expected to improve outcomes, and can pick up on tumour signals specific in ctDNA. These signals can include loss of heterozygosity, mutations on tumour suppressor genes (such as TP53) and oncogenes (such as KRAS). Another promising development includes the examination of the integrity of non-coding DNA repeat sequences, such as ALU and LINE1.
This offers multiple potential uses for diagnostics based on ctDNA, including:
- Cancer prognosis and detection
- Treatment response monitoring and treatment selection
- Estimating tumor size and location
The ability of ctDNA for detecting cancer, particularly in asymptomatic individuals, can revolutionize cancer diagnosis; it provides a clear advantage over traditional biopsies, especially when the location of the tumour cannot otherwise be determined. Its other uses in prognostics are based on multiple studies which establish ctDNA as a good predictor of future relapse and tumour aggressiveness. For example, a 230-patient study on colorectal cancer found that all individuals who tested positive for ctDNA subsequent to a tumour resection surgery relapsed within 3 years, unlike those without detectable ctDNA who only exhibited a 10% rate of relapse.
Biomarker Profiling and Treatment Response
Though the potential for improved and earlier diagnoses remains significant, the most promising use of ctDNA for clinical development remains the promise of understanding treatment response and biomarker profiling. Immuno-oncology has been experiencing revolutionary growth in innovating novel treatments that can provide truly significant life extensions, and even remissions. However, these therapies remain limited by low response rates. Linking responses to specific biomarkers will be pivotal as we seek to trial and develop new immunotherapies, as outlined in our recent interview with Jessica Rege from Alkermes regarding the future of immune checkpoint blockades.
The sheer amount of data required to narrow down the causative mechanisms of treatment response for immunotherapeutic agents can be daunting – and nearly limitless. Collecting this data requires frequent sampling – which is best done through biopsies. However, there is a limit to how much tissue can be collected and how often tissue biopsies can be performed – due to their invasive nature; not only are they resource-intensive, but they can also discourage participation and patient retention in trials.
The amount of ctDNA itself can act as a non-invasive biomarker, as can the other information revealed by sequencing ctDNA. Immunotherapies using ctDNA as a predictor have already made progress. A study in metastasized Non-Small Cell Lung Cancer (NSCLC) observed a strong positive correlation between treatment response with immune checkpoint inhibitors and decreases in ctDNA levels. ctDNA was also found to be one of the earliest signs of treatment response in metastatic breast cancer.
Future Trends
ctDNA has been a known phenomenon for many years – but has only begun gaining traction in recent times. This is due to the challenges in isolating and detecting the relatively low levels of ctDNA in the bloodstream, and distinguishing them from general cfDNA. Advancements in high-throughput next generation sequencing, such as nanopore sequencing from liquid biopsies, have made great strides in increasing the viability of ctDNA – both by reducing costs, increasing speeds and accuracy. This will prove particularly critical as we develop novel therapies that target abnormalities on EGFR, KRAS and BRAF. When developed properly, ctDNA assays can provide a more holistic understanding of the genomic profile of a tumour – as they provide a glimpse into multiple fragments of it. This is in contrast to tissue biopsies that provide a limited genomic profile specific to the region of the tumour that is sampled; this is even more true when multiple tumours are present.
Another avenue for future research would be the application of the same principles to circulating, cell-free mRNA (ccfmRNA), particularly non-coding microRNA (miRNA), to detect and analyze tumour-derived mRNA. RNA samples present unique challenges however, as they are less stable than DNA – resulting in an even lower abundance, a problem compounded by their possible contamination with cellular mRNA. Progress in this area is expected to be slower, due to the obstacles in deconvoluting meaningful biomarkers from mRNA collected in bodily fluids and sorting out the background noise.
We can therefore safely conclude that ctDNA is here to stay. The information it can provide is a natural fit for the trajectory of oncology, particularly immuno-oncology. As we innovate therapies that exploit unique tumour genetic profiles, a non-invasive approach to sampling tumour genomes at higher frequencies will be a big enabler. However, ctDNA by itself will not be adequate – immunotherapies also depend on a detailed understanding of the tumour microenvironment, and tissue biopsies will remain the best way to assess that for some time to come. But as sequencing technology advances and new bioinformatics methods to characterize ctDNA emerge, its prominence in clinical development will only increase.
Join Proventa International’s Oncology Strategy Meeting in Boston in 2022 to hear the latest developments in ctDNA and precision oncology from world-renowned experts. Seize the opportunity to meet key stakeholders in the area, and talk to potential partners and collaborators that can advance your own journey in the field.

Subscribe
to get our
LATEST NEWS
Related Posts

Immunology & Oncology
The Silent Guardian: How GAS1 Shapes the Landscape of Metastatic Melanoma
GAS1’s discovery represents a beacon of hope in the fight against metastatic disease.
Immunology & Oncology
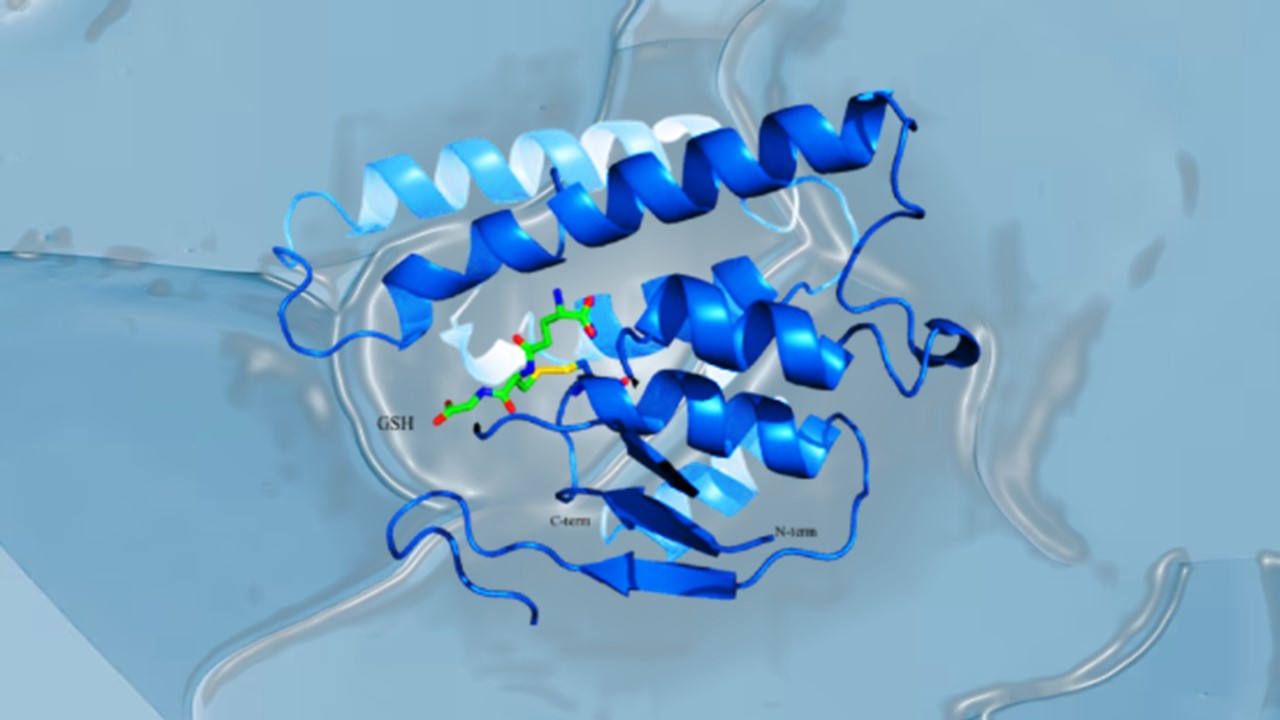
Resistance Mechanisms Unveiled: The Role of Glutathione S-Transferase in Cancer Therapy Failures
Understanding this dual role of GSTs as both protectors and accomplices to malignancies is central to tackling drug resistance.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.
Designing Better Sugar Stoppers: Engineering Selective α-Glucosidase Inhibitors via Fragment-Based Dynamic Chemistry
One of the most pressing challenges in anti-diabetic therapy is reducing the unpleasant and often debilitating gastrointestinal side effects that accompany α-amylase inhibition.